For any physician, calculating how much each patient is on the hook to pay is an essential part of running an efficient practice. Failing to do so properly and in a timely fashion can lead to confusion, frustration, and even legal issues if bills are left unpaid. Determining patient responsibility, therefore, is a task worth doing right.
This comprehensive guide helps healthcare providers learn how to calculate PATIENT RESPONSIBILITY in medical billing. But first, we will shed light on what patient responsibility is and why it’s important to calculate it as a provider.
What is Patient Responsibility in Medical Billing?
Patient responsibility is a portion of the medical bill a patient owes out-of-pocket. That means the patient must pay all their medical expenses with no health insurance plans. This includes deductibles, co-pays, and co-insurance amounts, all determined by the patient’s individual insurance plan.
For patients with high-deductible health plans, they have to pay heavily too, at first. Deductibles now average thousands per year. So any routine care, checkups, or minor health issues require full payment upfront by the patient. Insurance won’t pay one red cent until the patient has paid the deductible in full. The patient is on the hook for all costs at the outset. Only after paying through the nose will insurance finally kick in and share some of the burden.
Understanding patient responsibility is important for patients to make informed choices about their care and budget accordingly. And it’s equally critical for healthcare providers to ensure a smooth revenue cycle.
Importance of Understanding & Calculating Patient Responsibility
It’s important for providers to learn about the expected revenue so they can allocate resources for patient care and manage their finances accordingly. They can also make strategic decisions to up their bottom line in future.
By calculating accurate patient responsibility, healthcare providers also discover gaps in insurance coverage so they can collaborate with patients on alternative payment options and financial programs like Medicare, Extra Help, RxAssist, and more.
These are the quick benefits of understanding and calculating patient responsibility for healthcare providers:
- Get paid faster
- Less paperwork
- Happy patients because of the clear communication

As for patients, knowing what they owe upfront allows them to budget for healthcare costs and avoid surprise medical bills. Understanding their responsibility also helps choose the care that best fits their needs and budget. No more bill shocks for patients!
5 Factors Influencing Patient Responsibility
The amount a patient owes out-of-pocket can vary significantly depending on five key factors. Understanding these factors helps patients and providers to plan and direct the financial aspects of healthcare effectively.
- Insurance Coverage
- Deductible Amount
- Copays and Coinsurance
- Healthcare Service Type
- Patient’s Financial Situation
1. Insurance Coverage
The level of insurance coverage a patient has can greatly influence their out-of-pocket expenses for healthcare. Different insurance plans cover medical costs to varying degrees – some plans pick up most of the tab, while others leave the patient footing a larger portion of the bill.
For patients, more comprehensive coverage means less money coming directly out of their wallet to pay for treatment. This allows them to better plan for costs and not be caught off guard by expensive medical bills.
On the provider side, they can get a general sense ahead of time of what reimbursement to expect based on the patient’s insurance coverage. This helps providers map out their own finances and forecast revenue streams based on what the patient’s insurance company agrees to pay.
2. Deductible Amount
An important factor that determines a patient’s financial responsibility is the deductible amount set in their health insurance plan. The deductible is a pre-determined dollar amount patients must pay annually before insurance benefits kick in.
For the patient, an understanding of this amount allows for fiscal planning to cover medical expenses, avoiding surprise medical bills.
For the healthcare provider, knowledge of the deductible clarifies how much the patient owes, enabling the provider to collect the patient’s share efficiently.
3. Co-Payments
When a patient receives healthcare services, two key factors influence how much they will owe out-of-pocket: copayments and coinsurance.
Copayments, sometimes shortened to copays, are fixed dollar amounts that a patient pays when they receive a specific medical service. For example, a patient may have a $30 copay for a doctor’s visit or a $10 copay for a prescription medication. These copays are paid at the time of service.
Copayments allow patients to budget for predictable healthcare expenses, since the copay amounts are pre-set. Paying a flat copay upfront also discourages patients from unnecessary medical visits or services. For healthcare providers, copays supply some guaranteed revenue directly from the patient at the time of service.
4. Co-Insurance
Coinsurance refers to the percentage of costs that a patient pays for a healthcare service, after they have met their annual deductible. For instance, if a patient has 20% coinsurance and receives a $2,000 medical bill, they would owe $400 (20% of $2,000). The coinsurance applies once the deductible has been reached for the year.
Coinsurance links the patient’s financial responsibility to the overall cost and complexity of services. Since patients pay a percentage of the total charges, their out-of-pocket costs rise with more intense services. Coinsurance helps providers cover a portion of the total bill and limit losses from non-payment. It also reduces overuse of unnecessary services by patients.
5. Type of Healthcare Service
The nature of the service rendered can also influence patient responsibility. Specialist visits, diagnostic tests, or emergency room services often have higher co-pays or co-insurance percentages compared to routine check-ups or preventive care.
Understanding the type of medical services rendered by providers helps patients pre-calculate their responsibility and avoid surprises. And in the same way, providers will also learn how much to expect from a specific service.
6. Patient’s Financial Situation
Even small copays and deductibles offer a significant burden for patients with limited financial resources. As a provider, you must have open communication with patients and insurance companies. Get your patients to explore options for financial assistance programs or establish payment plans for them.
Understanding a patient’s financial situation helps providers have a clear idea of what and how to go ahead with the patient. And patients can also choose their insurance plans according to their financial situation.
How to Calculate Patient Responsibility as a Provider in Medical Billing
Determining patient responsibility starts at registration, verifying insurance details and potential coverage.
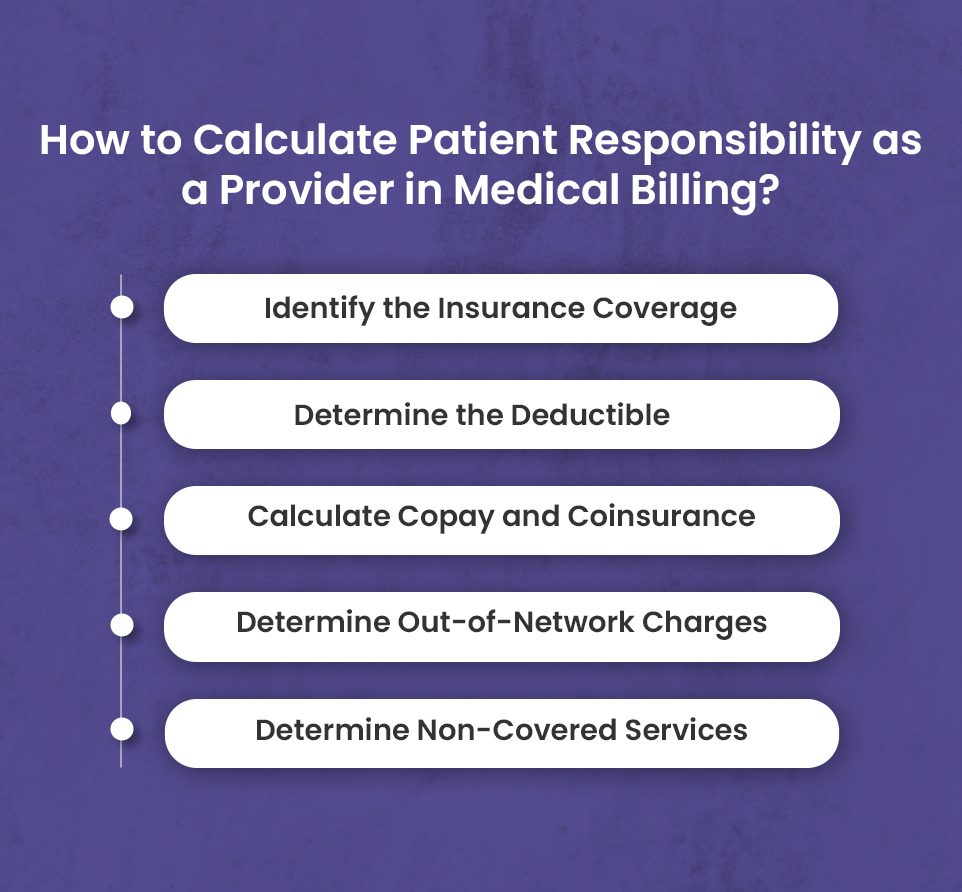
Step 1: Identify the Insurance Coverage
To figure out a patient’s financial responsibility, the medical provider has to start by looking over their insurance plan. They need the patient’s insurance card to get information like what kind of plan it is, the ID number, limits of coverage and any restrictions. For some treatments, the insurance company requires approval before the procedure can happen.
Once the doctor knows all the details about what the insurance covers, they can work out how much of the total charges the insurance will pay and how much the patient owes out of their own pocket. The provider uses all this information to determine the patient’s responsibility.
We do prior authorizations for each patient that visits your facility. Schedule free consultancy to know more.
Step 2: Determine the Deductible
To determine a patient’s deductible, first check their insurance card for the deductible amount and whether it’s for an individual or family plan. If it’s a family plan, find out how much of the deductible has already been met by other family members.
Next, look at the patient’s insurance company website to see their deductible details and year to date amounts applied. Call the insurance company directly if anything is unclear or not available online. A quick conversation can save hours of confusion and rejected claims.
Once you know the deductible amount and how much has been paid, calculating the patient’s responsibility is simple.
If the full deductible hasn’t been met, the patient owes the difference between what insurance will pay and the total charges for their care. Be sure to collect that amount at the time of service. It benefits the practice to have the patient pay their responsibility upfront to avoid billing them later.
After the deductible has been satisfied, the insurance company will typically pay a larger portion of the charges, leaving the patient with only a co-pay or coinsurance amount for each visit.
By determining the deductible at the beginning, you have a clear understanding of what the patient owes for each visit and can collect the proper amount, allowing you to receive payment in a timely manner for the services you provide. This simple process of checking details upfront creates a smooth experience for both the patient and the practice.
Step 3: Calculate Copay and Coinsurance
When providers send bills for medical services, determining what the patient owes out-of-pocket involves a couple key factors. There’s the copayment, a flat fee paid per office visit or prescription. Like if Mary has a $30 copay for seeing her doctor, she’ll owe $30 at the time of the appointment regardless of the total bill.
Then there’s coinsurance – the patient’s share of costs calculated as a percentage. For example, if John’s knee surgery is $10,000 and his plan has 20% coinsurance, he’ll owe 20% of $10,000, or $2,000.
- By first collecting the copayment, then calculating and billing for coinsurance, providers can figure out the patient’s payment responsibility.
In some cases, coinsurance and copay appear together for a patient. They would pay the copay upfront, and then the coinsurance percentage would be applied to the remaining balance.
Step 4: Determine Out-of-Network Charges
Navigating patient financial responsibility for out-of-network medical charges can be an intricate process, but providers can take certain steps to make appropriate determinations.
The provider must first gather information on the patient’s insurance coverage to understand what is considered in-network versus out-of-network. This often requires calling the insurance company directly to inquire about the patient’s plan details. It is important to document any information received, including applicable deductibles, copays, and coinsurance rates.
With this knowledge in hand, the provider can now determine their full charges for the services rendered to the patient. These standard charges act as the starting point. The provider must then discount the charges based on any negotiated rates established with the patient’s insurance company. If no negotiated rate exists, the full charges stand.
The resulting out-of-network fee amount must be clearly conveyed to the patient upfront, ideally in writing. This allows the patient to make an informed decision on receiving care.
From here, the patient’s portion of responsibility depends on their plan benefits. Any deductible or coinsurance owed will be applied to the out-of-network fee at the percentages dictated by the insurance company. The provider can collect this amount directly from the patient.
Handling out-of-network charges in this manner allows the provider to receive fair compensation while giving the patient full transparency into costs. Though time-consuming, it is the most equitable way to operate. The provider upholds their financial interests while also providing excellent service to patients, no matter their insurance circumstances.
Step 5: Determine Non-Covered Services
Non-covered services are services for which patients are required to pay in full, on their own. They are, after all, not covered by insurance companies.
For example, Medicare never covers certain services like foot care or preventive examinations like routine physical check-up, represented by CPT codes 99381-99397. These services are usually not medically necessary.
Look up the patient’s insurance plan and confirm the medical necessity of a service to determine the non-covered services.
Streamline Patient Responsibility with BellMedEx’s Medical Revenue Service
Calculating patient responsibility is a necessary evil for providers, but our company’s sole focus is to lift this burden. We put medical practices on autopilot by taking on the patient liability estimation that burns up provider time and energy.
Our sophisticated process gathers all the necessary details – from payer contracts to patient benefits – to determine the most accurate responsibility estimate possible. This protects providers from undercharging patients and losing revenue. The end result is more time for providers to devote to patients, less administrative hassle, and optimized revenue collection.
Contact us today to implement our complete medical revenue service, including unparalleled patient responsibility calculation.