Medical Coding Services
Best Medical Coding Solutions. No Revenue Leakage, Get Paid On-Time.
- Providers receive timely payment.
- Patients are accurately billed for services
- Payers accept claims without rejection.
Schedule Online Appointment:

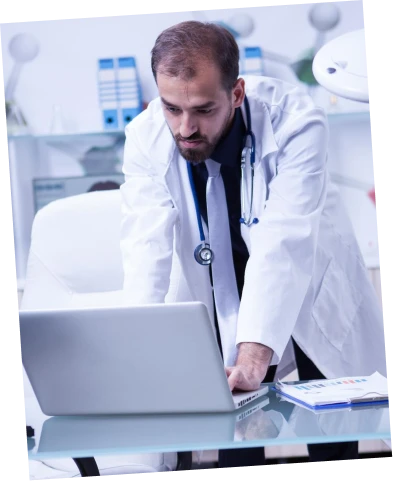
How does BellMedEx Medical Coding Company help?
Clinical Statement Analysis
Our coders carefully analyze medical statements and documentation provided by healthcare providers. They classify this information using standardized classifications.
Medical Notes Coding
Physician coders convert diagnosis procedures into codes that are easily readable by insurance companies and hassle-free for medical providers.
Super-Bill Submission
Our coders work with the billing team to generate a super bill that includes charges the payer is responsible for patient insurance coverage, and any co-payments.
Claim Approval
Our coders advocate for the healthcare provider to ensure the claim is approved. They work to recover Aged Receivables and help ensure that denied claims are paid.

Why Choose BellMedEx Coding Agency?
Accurate medical coding has become a necessity, particularly since ACA law has obligated healthcare providers to furnish patients with medical services they receive along with their corresponding expenses.
At BellMedEx, our certified coders analyze medical records to assign the proper standardized codes. This clinical coding expertise ensures your claims are reimbursed fully and quickly. No more submitting a service only to wait months for payment because of a coding error.
We follow the latest medical coding guidelines and legislation so your claims comply. This protects you from audit risks and overcharging patients due to unbundling. With BellMedEx, your reimbursements will be timely and accurate.
Our rigorous training and continuing education gives our coders an edge. They identify the right codes for even the most complex cases. This clinical coding solution helps avoid those claim denials that lead to revenue loss.
Put BellMedEx’s medical coding services to work for your practice. Our clinical coding solutions bring speedy and correct reimbursements in today’s climate of growing regulations. Outsource your coding needs and gain peace of mind knowing claims are coded right the first time.
Try our affordable medical coding service that pays for itself...
Our medical coding and auditing recovers revenue that you're currently missing. The increased reimbursement will more than cover our reasonable fees.
- Certified coders
- Ongoing audits
- Detailed reporting
- Rapid turnaround
Hire AHIMA & AAPC Certified Medical Coding Experts
BellMedEx medical coding experts analyze patient records and assign diagnosis + procedure codes to them with 99% accuracy. This CPC coding helps healthcare providers receive proper reimbursement from insurance companies. Our skilled coding managers thoroughly review all charts to ensure compliance with ICD-10, CPT and HCPCS standards. You can trust BellMedEx to capture every diagnosis, test, and treatment with the right codes for optimal revenue cycle management.


Custom coding solutions for every healthcare facility
Unlock billing via medical coding and documentation services
BellMedEx medical coding service relies on specialized software that scans medical records and provides an initial set of suggested codes. Our medical coders then review the records, analyze the suggestions, and finalize the codes based on their in-depth understanding of coding rules. This audit results in highly accurate coding that translates health records into the proper billable codes insurance companies require.

Get medical coding done right with our proven process
Here’s our systematic approach to represent patient diagnosis documentation within the codes.
Clinical coders encode medical charts into numerical and letter coded data string sequences.
Assignment process finds the relevant codes from the medical classification and entering it into the data collection system.
Clinical coders review medical codes to ensure accuracy, including the diagnosis-related group (DRG) if financed via case mix prototype.
Medical billing advocates work with payers to ensure fair reimbursement for healthcare providers, resolving any issues with denied claims.
Medical coding team ensures timely payment by closing tickets only after payment and claims acceptance.
BellMedEx ICD-10 Medical Coding Services & Solutions 2024
Facility Coding Service
Getting facility services paid ain’t easy. Atleast, not without experts who know the codes. BellMedEx’s medical coding department has the HCPCS know-how to get it right. We take all your inpatient services – the wheels, the rooms, the nursing – and code them properly. Contact us now to avail facility coding service.
Professional Fee Coding Service
The doctor sees the patient. The doctor does tests. The doctor prescribes medicine. But then what? That’s where BellMedEx comes in. Our pro fee coders get the doctor paid right. We make sure the insurance company pays the doctor fair. The patient sees a correct bill too. No surprises. Contact us today for profee coding service.
Payer Specific Coding Service
Each payer has their own way of accepting codes. This can confuse doctors. But our coders know the rules of big payers. Like UnitedHealth, Cigna, and Humana. Our team works as per the guidelines for each payer’s codes. This way, claims process smoothly and doctors get paid without unfair cuts. Contact us today to avail coding solutions for your payer network.
Offshore Coding Service
Do you want to save your medical coding budget? With BellMedEx offshore coding service, medics receive high-caliber coding at a lower price point. We identify and develop coding talent overseas, where pay standards are more affordable. Your coding gets done for a fraction of the cost, following all HIPAA rules. Contact us today for offshore coding solutions.
General Practitioner Visits Coding Service
Getting paid for seeing patients. That’s what GP visits coding does. We make sure your claims get approved. So the cash keeps flowing into your practice. Our expert coders know all the codes by heart. They get it right the first time, every time. Contact BellMedEx now to learn more about our coding service for general practitioners.
Outpatient Coding Service
HCC Coding Service
Inpatient Coding Service

Are You Frustrated with Medical Coding Errors, Denials, and Delays?
BellMedEx provides complete medical coding solutions and services. Our certified coders handle all coding projects — in patient, outpatient, emergency, or specialty services. So don’t let medical coding problems affect your bottom line, as our experts will detect them and correct them before they damage your practice.
BellMedEx Coding Audits & Consultancy Solutions
Our consultancy services help prevent lost revenue from coding errors.
Code Audits
Trust our coding auditors to validate your records, maximize revenue, and keep you compliant with regulations. Our experts find issues, fix errors, and optimize your codes.
Documentation Review
Documentation holds the keys to coding. Our review unlocks accuracy, capturing every revenue dollar while averting audit risks.
Coding Consultancy
Our coding consultants dive deep into patient charts to apply the right codes, enabling proper reimbursement and a clear view of population health.
Let's transform your medical records into fair revenue...
Our dedicated medical coding experts efficiently extract insights from patient data to maximize your reimbursements.
- Skilled Coders
- HIPAA Compliant
- Improved Cash Flow
- Reduced Denials
BellMedEx Coding by the Numbers
Keeping Patient Data Safe
BellMedEx is a medical coding solutions provider that values the security and confidentiality of your patient data. That is why we adhere to the HIPAA standards and use the latest encryption, firewall, antivirus, and other security technologies to protect patient’s data from any unauthorized access, use, or disclosure. We have obtained various certifications, such as SOC 2 Type 2, ISO 27001, ISO 9001, and KLAS/Censinet Cybersecurity Transparency, to demonstrate our commitment to security, quality, and transparency in our medical coding services.


Medical Coding Solutions that Meet Compliance Needs
BellMedEx Medical Coding Solutions follow the HIPAA Privacy Rule and the HIPAA Security Rule for the collection, storage, transmission, and disposal of protected health information (PHI). We comply with all the US government healthcare data regulations, such as the Medicare Access and CHIP Reauthorization Act (MACRA), the Merit-based Incentive Payment System (MIPS), the Medicare Shared Savings Program (MSSP), the Comprehensive Primary Care Plus (CPC+), and the Quality Payment Program (QPP). In addition, our staff receives regular training for the latest changes in HIPAA, GDPR, CMS Fraud, Waste and Abuse, ISO 27001, and Social Engineering topics.
Get advanced help with Medical Coding

0% Staffing Burden
Don't stretch your staff thin with coding. Our service analyzes records and assigns precise codes for you. No need to hire, train and manage additional in-house coders. Outsource to us and reduce staffing burdens.
Complete Denial Assistance
Stop losing hard-earned income. Our coders' hawk eyes spot deficiencies leading to denials. We optimize records so you get paid for all you do. No more lost revenue.

Reduction in DNFB and Backlogs
Backlog refers to the number of cases pending to be coded after discharge. DNFB refers to the ratio of accounts that are not final billed due to incomplete or inaccurate coding or documentation. BellMedEx eliminates the backlog of uncoded cases and decreases DNFB ratio.
Practices thrive when records reflect the whole patient. Contact us today for medical coding audits and consultancy!
BellMedEx offers Modern Coding Solutions for the American Healthcare System, like:


Managing Overlook for Coding (OFC)
This is a proprietary algorithm that we use to measure and manage the productivity and quality of our coding team. It allows us to monitor the coding process in real-time, identify and correct errors, and generate reports and analytics.

Calculating Risk Adjustment Factor (RAF) Score
This is a measure of the expected health care costs for a patient based on their diagnoses and demographic factors. A higher RAF score indicates a higher risk and complexity of the patient’s condition. We use our expertise in coding and documentation to ensure that your RAF scores accurately reflect the severity of your patient population and maximize your reimbursement from Medicare Advantage plans.

Improving Discharged Not Final Billed (DNFB) Rate
This is a proprietary algorithm that we use to measure and manage the productivity and quality of our coding team. It allows us to monitor the coding process in real-time, identify and correct errors, and generate reports and analytics. It allows us to monitor the coding process in real-time, identify and correct errors, and generate reports and analytics.

Managing Discharged Not Finally Coded (DNFC) Cases
This is the number of days a case remains before being finally coded after discharge. A high DNFC can delay your claim submission and reimbursement, as well as increase your coding backlog and workload. We help you lower your DNFC by providing fast and affordable coding services, using our OFC software and our skilled coders.
Optimizing Diagnosis-Related Group (DRG)
This is a system that classifies hospital cases into groups that have similar clinical characteristics and resource use. Each DRG has a relative weight that reflects the average cost of treating a patient in that group. DRGs are used by Medicare and other payers to determine the payment rates for inpatient hospital services. We help you optimize your DRG assignment by applying our knowledge of the MS-DRG system, the coding rules, and the documentation requirements.

Increasing Case Mix Index (CMI)
This is the average relative weight of the diagnosis-related groups (DRGs) for all patients treated at your facility. A higher CMI indicates that you have treated more complex and resource-intensive patients, which may result in higher reimbursement rates from Medicare and other payers. We help you improve your CMI by assigning the most appropriate DRGs for your cases, based on the ICD-10-CM and PCS codes and the MS-DRG system.
Don't Let Medical Coding Errors Cost You Your Revenue.
BellMedEx Medical Coders Are Here To Serve You!
BellMedEx offers the best solutions for all medical coding challenges. Our clinical coders gracefully handle any specialty and volume of coding. We use the latest EHR technology to ensure compliance. We also provide physicians with transparent reports to monitor their coding performance and revenue cycle.
