Need help with CCM coding?
I am here for you. Let’s talk!
Chronic care management plays a vital role in the healthcare industry, especially for common chronic diseases.
Almost 129 million people in the US suffer from at least one major chronic disease. This significantly impacts their lives and contributes to a large portion of healthcare costs.
In addition, nearly 90% of the annual budget (which totals $4.1 trillion) goes to treating chronic diseases and mental health conditions.

People can enhance their overall quality of life by keeping up with regular check-ups and managing their medications.
The Center of Medicaid and Medicare Services (CMS) has established standard CPT codes to facilitate medical billing and reimbursement for Chronic Care Management (CCM) services. Healthcare professionals find these codes helpful for recording the time and effort spent on all CCM activities.
This blog provides an overview of CPT codes and billing guidelines for CCM.
Chronic Care Management CPT Codes
Chronic Care Management (CCM) codes help physicians get paid for managing patients with chronic conditions. These codes capture the non-face-to-face care coordination services furnished to Medicare beneficiaries, such as communication with the patient and caregivers, medication management, and remote monitoring of health conditions.
The CCM codes fall into two categories: complex and non-complex chronic care management.
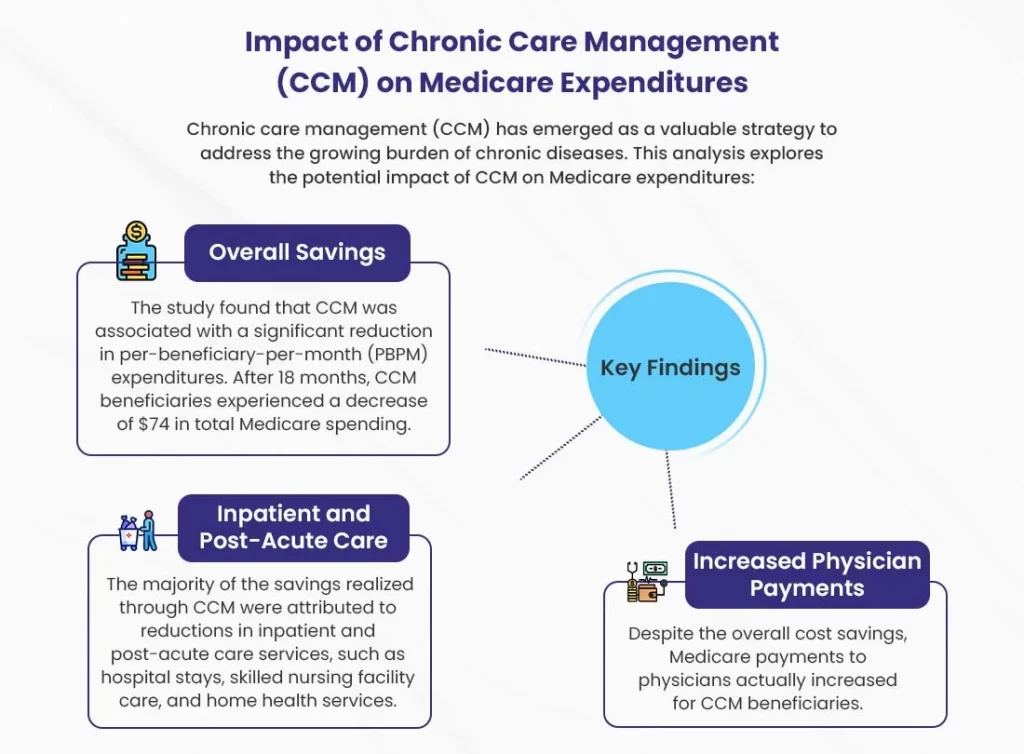
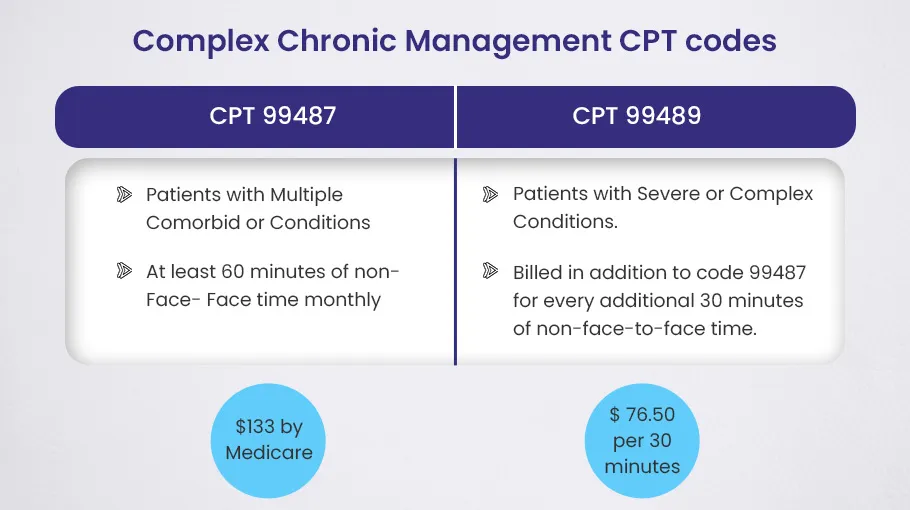
➜ The complex CCM codes, 99487 and 99489, describe care for patients with multiple chronic conditions that pose a significant threat to health or psychosocial status and require comprehensive care plan oversight.
➜ The non-complex CCM codes, 99490 and 99491, are for patients with two or more chronic conditions that are expected to last at least 12 months or until the death of the patient, but do not require the intensive management of complex CCM codes.
Medicare uses these CCM codes to pay separately for non-face-to-face care coordination services. This helps physicians improve care for beneficiaries with multiple chronic conditions.
COMPLEX Chronic Care Management CPT Codes
Complex chronic care management codes (CCMC) are specialized medical billing codes used by healthcare providers to report non-face-to-face care coordination and management for patients with multiple chronic conditions. Physicians and care teams employ these codes when a patient’s condition requires extensive management and monitoring due to the severity and complexity of their illness.
To report CCMCs, physicians must spend at least 60 minutes of qualified time per calendar month providing care coordination, monitoring patient conditions, adjusting treatment plans, and ensuring patients have access to necessary healthcare resources. The time spent reviewing medical records, communicating with other physicians, patient education, and arranging referrals and procedures are all considered qualified time.
Complex Chronic Care Management CPT Codes include:
CPT Code 99487
| Used For | Patients with multiple chronic conditions (comorbidities) requiring significant care coordination. |
| Timings | Clinical staff must spend at least 60 minutes per month on non face-to-face care coordination. |
| Reimbursement | Medicare reimburses $133 per month for each patient receiving complex care. |
CPT code 99487 is for what’s called “Complex Chronic Care Management.” It’s used for patients who have multiple chronic conditions all at the same time – what doctors call “comorbid conditions.” These are serious illnesses that need a good deal of care and time to manage properly.
Now, for this CPT code to apply, the clinical staff at the doctor’s office or healthcare practice has to spend at least 60 minutes per month on non face-to-face care coordination for the patient. So lots of time on the phone or doing paperwork – whatever it takes to get that patient the care they need from all their different doctors. Medicare will reimburse the practice $133 per month for each patient getting this complex care.
Some examples of conditions that would qualify someone for the 99487 code are things like arthritis, heart disease, COPD, and high blood pressure. But it’s not limited to just those. The main thing is the patient has multiple ongoing illnesses that all need management at the same time.
Let me give you an example of how this might look for a real patient:
Say someone has type 2 diabetes, heart failure, and chronic kidney disease all together. To give them the best care, you’d need to monitor their blood sugar, blood pressure, and kidney function continuously. And you’d likely need a whole team of specialists like nephrologists, endocrinologists, and cardiologists to make a comprehensive treatment plan. The 99487 code helps make sure caring for patients with these complex chronic conditions is feasible for healthcare practices.
CPT 99489
| Used For | Patients with severe or life-threatening illnesses requiring extensive care coordination. |
| Timings | Care team must spend at least 30 minutes beyond regular chronic care management codes for each 99489 billing. |
| Reimbursement | Medicare reimburses $76.50 for each 30 minutes billed under 99489. |
CPT code 99489 is for complex chronic care management of patients with severe conditions. This code is for when a patient has a really bad illness – think end stage kidney failure, or advanced heart disease, or some neurological disorder that has them all messed up. These patients need a lot of care and time from their healthcare team to manage all their needs. The doctor and nurses have long talks about the best treatments, how to handle side effects, what to expect down the road, and how to keep spirits up when the road ahead is rough.
To bill 99489, the care team has to spend at least 30 minutes beyond the regular chronic care management codes working on the patient’s case. And they can keep adding 99489 for each extra 30 minutes they spend coordinating care, reviewing labs and records, talking to specialists, and having those long empathetic chats about options and quality of life that these complex cases need. Medicare reimburses $76.50 for each 30 minutes billed under 99489.
Let’s imagine a scenario. Say there’s a man with early stage pancreatic cancer. He’s gotta have frequent visits to weigh multiple treatment options, figure out palliative medicines for the pain and nausea he’ll likely get, and talk over hospice care down the line. His care team talks through all this with him and his family, being there for emotional support too. For all that non-face-to-face time spent managing his complex condition, the doctor can bill 99489.
CPT Code 99487 vs CPT 99489
| Complex CCM CPT Codes | Used For | Timings | Medicare Reimbursement Rate |
| CPT 99487 | Patients with Multiple or Comorbid Conditions | At least 60 minutes of non-face-to-face time monthly | $133 by Medicare |
| CPT 99489 | Patients with Severe or Complex Conditions. | Billed in addition to code 99487 for every additional 30 minutes of non-face-to-face time | $76.50 per 30 minutes |
NON-COMPLEX Chronic Care Management CPT codes
Non-complex Chronic Care Management (CCM) CPT codes are used to report non-complex services given to patients with chronic conditions. These codes help healthcare providers accurately record the time and services provided for managing chronic patients who do not qualify for complex CCM.
A doctor or qualified healthcare worker needs to spend at least 20 minutes each month on care activities for the patient with simple CCM. These tasks can involve looking over patient records and test results, talking with other health care workers who are part of the patient’s care, teaching patients and their families, and creating, putting into action, and updating care plans.
Non-complex CCM codes can be billed once a month for patients who have two or more ongoing health issues that are likely to last at least a year or until the patient’s death.
To bill for non-complex CCM, the practice needs to have a patient already established and a care plan ready. They must offer 24/7 access to care and ensure continuity of care. It’s important to carry out regular assessments of the patient’s medical, functional, and psychosocial needs, and provide care management services guided by a physician or another qualified healthcare professional.
Non-complex Chronic Care Management CPT Codes include:
CPT 99490
| Used For | Medicare patients with two or more ongoing health issues requiring continuous medical attention. |
| Timings | Clinical staff must spend at least 20 minutes per month on non face-to-face care coordination. |
| Reimbursement | Medicare reimburses $62 per patient per month. |
CPT code 99490 covers at least 20 minutes per month of non-face-to-face time spent by clinical staff providing care management to Medicare patients with two or more ongoing health issues requiring continuous medical attention. For their services, Medicare reimburses the provider $62 per patient per month.
CPT 99490 applies in cases such as a Medicare patient coping with both hypertension and asthma at the same time. Managing the blood pressure and lung function for an individual with these chronic diseases takes regular monitoring, medication adjustments, and lifestyle recommendations from their healthcare team. By using 99490 for chronic care management, the provider gets paid for the behind-the-scenes work involved in keeping complex patients as healthy as possible.
So in summary, CPT code 99490 offers a way for providers to receive compensation for the extra time needed to coordinate care for Medicare patients with multiple chronic conditions. It covers a 20 minutes minimum per month of non-face-to-face chronic care management services. For a patient battling both high blood pressure and asthma, for example, 99490 would pay for the medical team’s ongoing work guiding their treatment plan.
CPT 99439
| Used For | Patients with one or more ongoing health conditions requiring continuous tracking, but less complex than those qualifying for 99490 or 99487. |
| Timings | For each additional 20 minutes of non-face-to-face care coordination services beyond the initial 99490. |
| Reimbursement | Medicare reimburses $47 for each 20-minute increment. |
The CPT code 99439 is for chronic care management of patients with one or more ongoing health conditions that need continuous tracking. It is used when the patient’s situation is less complex or severe than what would call for the codes 99490 or 99487.
Specifically, 99439 is for each additional 20 minutes of non-face-to-face care coordination services when the initial code 99490 has already been billed. Medicare reimburses $47 for each 20-minute increment.
This code covers things like regular patient contact and medication reviews to ensure proper disease management. It is for the ongoing supervision of care, not just responding to issues as they arise. The goal is to prevent exacerbations and complications through vigilant monitoring and care planning.
For instance, take a diabetes patient who needs daily blood sugar checks and consistent advice about diet, exercise, and insulin dosing. The work involved in providing structured self-management support falls under 99439. This code helps cover the time spent enabling the patient to stay as healthy as possible.
CPT 99491
| Used For | The first face-to-face visit with a Medicare patient who has one or more chronic conditions. |
| Timings | At least 30 minutes of face-to-face time with a doctor or qualified healthcare worker. |
| Reimbursement | Medicare reimburses $83 for the initial visit. |
CPT code 99491 for chronic care management is used when a doctor or qualified healthcare worker spends at least 30 minutes in a face-to-face visit with a Medicare patient who has one or more chronic conditions. It’s for the patient’s first visit. Medicare reimburses the practice $83 for this initial chronic care management visit.
So in plain terms, 99491 is a billing code that doctors use to get paid for the first monthly visit with a Medicare patient who needs ongoing care for chronic illnesses like diabetes, COPD, or heart disease. The visit has to be at least 30 minutes of facetime with the doctor or nurse practitioner. And Medicare pays the clinic $83.
To understand how this CPT code works, let’s look at a hypothetical patient example. Say we have a 68-year-old woman with diabetes, high blood pressure, and arthritis – three chronic conditions. She comes to see her primary care doctor for the first time to set up a care management plan. The doctor spends 35 minutes with her, talking about all three conditions, adjusting medications, setting diet and exercise goals, and mapping out a schedule for follow-up visits and coordination with specialists.
In this case, after the visit, the doctor would bill Medicare using CPT code 99491, since this was the initial face-to-face chronic care management visit for this patient with multiple chronic diseases. And Medicare would reimburse the practice $83.
CPT 99437
| Used For | Subsequent face-to-face visits with patients who have chronic care management needs beyond the initial 60 minutes. |
| Timings | For each additional 30 minutes of face-to-face time. |
| Reimbursement | Medicare reimburses $21.88 for each additional 30 minutes. |
The CPT code 99437 is used for subsequent visits for patients with chronic care management needs. This code allows physicians to bill for additional 30 minute increments of face-to-face time beyond the initial 60 minutes covered by code 99491. Medicare reimburses $21.88 for each additional 30 minutes billed under 99437.
This code applies well for patients like Anna Leigh, who suffers from diabetes, hypertension, and obesity. These chronic conditions require regular monitoring and care coordination between visits. During a follow-up appointment, Anna’s physician may spend 45 minutes reviewing his blood sugar logs, adjusting medications, providing health education, and communicating with his endocrinologist. The initial 60 minutes would be covered under 99491. The extra 15 minutes of face-to-face time would be billed using 99437.
Billing code 99437 for subsequent chronic care management encounters enables physicians to receive payment for the additional time needed to properly coordinate care for patients with multiple chronic illnesses. This supports high quality, patient-centered care. The CPT guidelines require detailed documentation showing the additional time spent on chronic care management during each visit billed under this code. When used appropriately, 99437 provides fair compensation to physicians providing ongoing care to complex patients like Anna.
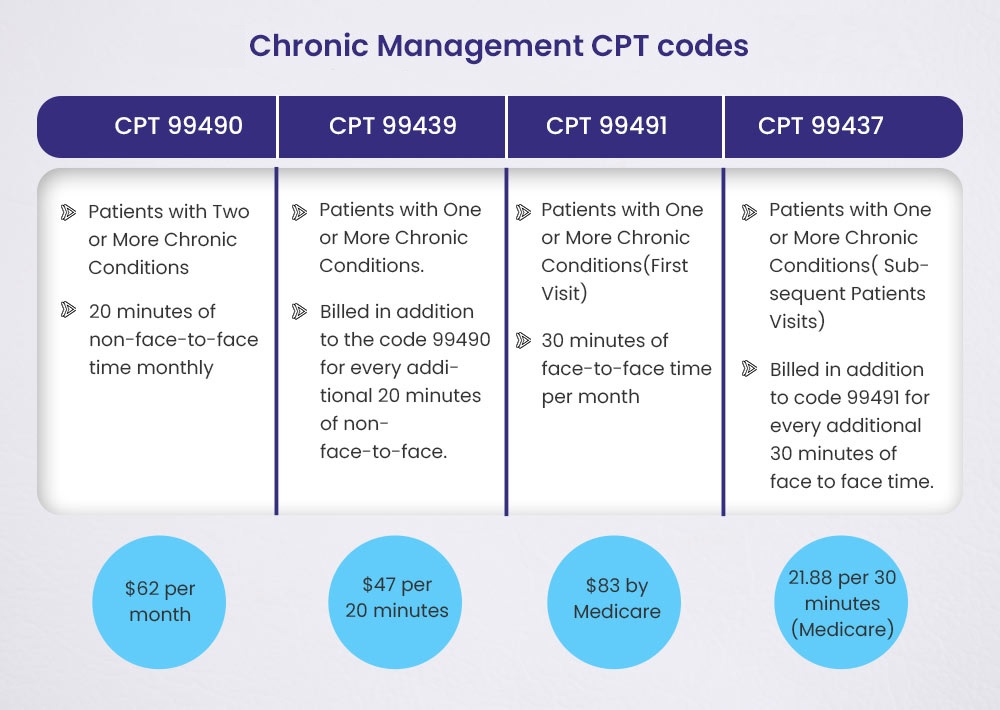
CPT Code 99490 vs 99439 vs 99491 vs 99437
| Non-Complex CCM CPT Codes | Used For | Timings | Medicare Reimbursement Rate |
| CPT 99490 | Patients with Two or More Chronic Conditions | 20 minutes of non-face-to-face time monthly | $62 per month |
| CPT 99439 | Patients with One or More Chronic Conditions | Billed in addition to the code 99490 for every additional 20 minutes of non-face-to-face | $47 per 20 minutes |
| CPT 99491 | Patients with One or More Chronic Conditions (First Visit) | 30 minutes of face-to-face time per month | $83 |
| CPT 99437 | Patients with One or More Chronic Conditions ( Subsequent Patients Visits) | Billed in addition to code 99491 for every additional 30 minutes of face to face time | 21.88 per 30 minutes |
💡 Note: The real rate of reimbursement for the CPT code of CCM may be different in each area. Always check the Physician Fee Schedule (PFS) to see the most recent payment rates.
BellMedEx: Your BFF for Chronic Care Management Coding! 🌠
We’re the coding superheroes who thrive on deciphering complex codes like 99490, 99439, and 99491, plus all those pesky time requirements.
Application Rate of High-Volume Chronic Care Management CPT Codes
Chronic care management (CCM) services are becoming increasingly important as our population ages and more patients suffer from multiple chronic conditions. Proper coding of these services is essential for practices to receive reimbursement and continue providing high-quality care.
Recent data reveals interesting trends in the utilization of common CCM CPT codes.
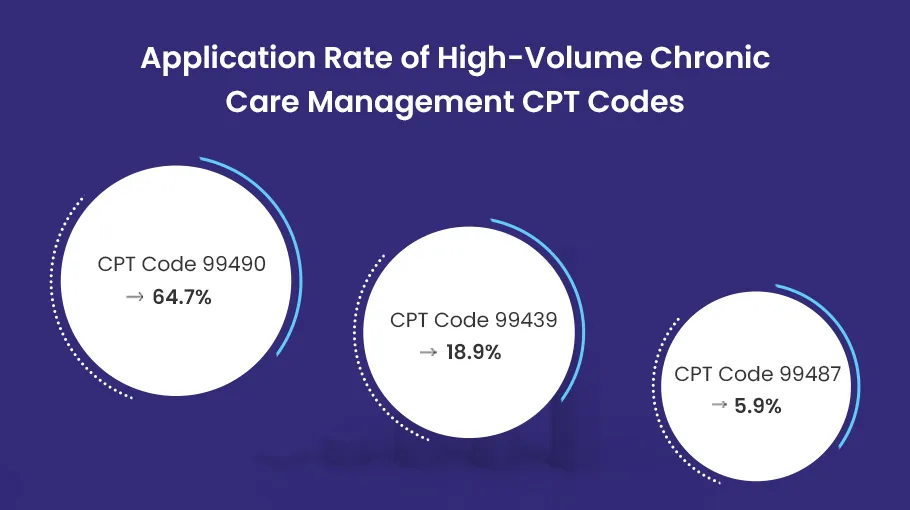
1️⃣ ➜ The most widely used code is 99490, for at least 20 minutes of non-face-to-face chronic care management services per month. This code accounted for 64.7% of reported CCM services. This high rate shows the demand for basic CCM services to coordinate care for chronically ill patients.
2️⃣ ➜ The second most used CPT code was 99439, for each additional 20 minutes of chronic care management services in a calendar month. At 18.9%, this demonstrates many patients require more than the initial 20 minutes allowed under code 99490. Complex patients benefit from additional time spent on care planning, medication management, and care coordination.
3️⃣ ➜ Rounding out the top three was code 99487, for complex chronic care management services requiring 60 minutes per month. While utilized less frequently at 5.9%, this code is rapidly increasing as practices take on more patients with multiple comorbidities needing intensive management.
| CPT code | % of total procedures |
| 99490 | 64.7% |
| 99439 | 18.9% |
| 99487 | 5.9% |
| 99491 | 3.3% |
| 99489 | 2.8% |
| 99437 | 0.3% |
The popularity of these codes underscores the value of CCM services. With rising chronic disease burden, CCM provides continuous proactive care between office visits. Tracking utilization of these codes over time will show if care management services are keeping pace with population needs. Wise use of CCM codes allows practices to be reimbursed for this vital non-face-to-face care coordination.
What Conditions/Diagnoses Need to Qualify for Chronic Care Management (CCM)?
✅ To qualify for the CCM program, patients must have at least two chronic conditions that require ongoing medical care and management for at least 12 months or until the end of life.
✅ The chronic conditions should be severe enough to potentially lead to functional decline, acute exacerbation/decompensation, or a life-threatening event if not properly managed.
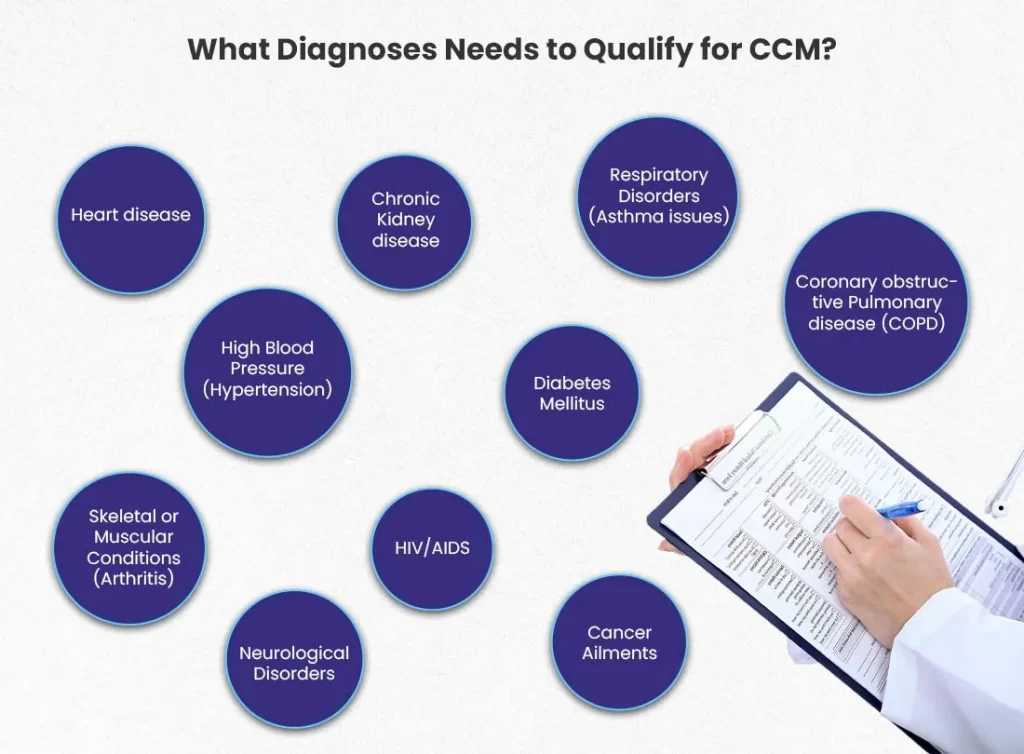
Some common chronic conditions that often qualify for CCM include:
- Cardiovascular diseases (e.g., heart failure, coronary artery disease)
- Respiratory diseases (e.g., COPD, asthma)
- Metabolic disorders (e.g., diabetes, hyperlipidemia)
- Neurological conditions (e.g., Parkinson’s disease, multiple sclerosis)
- Chronic kidney disease
- Alzheimer’s disease and other dementias
- Autoimmune disorders (e.g., rheumatoid arthritis, lupus)
- Cancer (active or in remission)
- HIV/AIDS
- Mental health conditions (e.g., major depressive disorder, bipolar disorder)
💡 Note: The above list is not exhaustive, and other chronic conditions may also qualify for CCM if they meet the criteria of requiring ongoing medical management and monitoring. The key factor is the presence of multiple chronic conditions that significantly increase the risk of functional decline, acute exacerbations, or life-threatening events if not properly managed through coordinated care.
Chronic Care Management Billing Guidelines
The CCM billing guidelines outline requirements providers must meet in order to bill for these important services. This includes details on eligibility, required services, consent, and billing specifics. This section will provide an overview of the CCM billing guidelines as outlined by CMS and commercial payers. It will cover requirements around eligibility, patient consent, scope of services, time thresholds, billing codes, and reimbursement to help practices appropriately bill for CCM services.
Key Requirements for Billing Chronic Care Management (CCM) CPT Codes
Managing billing for Chronic Care Management (CCM) services requires careful attention to key requirements. As outlined in the Medicare Learning Network (MLN) guidance, both complex and non-complex CCM codes have specific elements for appropriate billing:
- Initiation Through a Face-to-Face Visit — A qualifying visit with the billing practitioner lays the groundwork for CCM services. This visit establishes the patient’s consent, ensures they meet eligibility criteria, and begins care planning.
- Non Face-to-Face Services — CCM codes cover remote care coordination, not direct patient contact. Time spent on non face-to-face care management activities like phone calls, chart review, care plan oversight, and team conferences counts toward time requirements.
- Written or Verbal Consent — Patients must provide their agreement to receive CCM services, which is documented by the billing practitioner. Consent can be obtained at the initiating visit or separately.
- Certified Billing Practitioner — To bill CCM codes, the provider must be the one who furnishes and oversees the patient’s care management. Nurse practitioners, physician assistants, and clinical nurse specialists can provide CCM services.
- Patient Eligibility — CCM services are for patients with multiple (two or more) chronic conditions expected to last at least 12 months or until death, and that place the patient at significant risk of death or functional decline.
- Minimum Time Requirement — Both complex and non-complex CCM codes have a minimum time spent on care coordination activities per calendar month that must be met to qualify for billing.
- General Supervision of Auxiliaries — The billing practitioner provides general oversight of any clinical staff involved in delivering CCM services. Auxiliary personnel do not bill independently.
Closely following CCM billing rules ensures claims are submitted accurately and patients receive comprehensive, coordinated care management.
Requirements for Submitting Chronic Care Management Claims to CMS
Correct and comprehensive patient documentation is essential for filing clean claims. Healthcare providers need to present a complete collection of data in order to prevent denials. Below is an extensive checklist to help with the CCM claim submission procedure.
1). Patient Eligibility
To qualify for Chronic Care Management (CCM) services and submit claims to the Centers for Medicare & Medicaid Services (CMS), patients must meet specific eligibility criteria. CCM aims to provide comprehensive care coordination and management for individuals with multiple chronic conditions, ensuring they receive proactive, personalized care to improve their overall health outcomes.
The key requirements for patient eligibility are as follows:
☑️ ➜ The patient must be under the care of a qualified healthcare provider, such as a physician, nurse practitioner, or physician assistant.
☑️ ➜ The patient must have a significant risk of functional decline or mortality within the next 12 months due to their chronic conditions.
☑️ ➜ The patient must have two or more chronic conditions that require ongoing management and monitoring, including medications, therapy, or other interventions.
Additionally, it is important to note that:
- The healthcare provider must establish a comprehensive care plan for the patient, addressing all health issues and outlining treatment goals.
- The patient (or their authorized representative) must provide consent to receive CCM services and agree to the associated cost-sharing responsibilities.
- The healthcare provider must document all CCM activities, including care coordination, medication management, and communication with the patient and other healthcare professionals involved in their care.
2). Documentation of Care
A comprehensive patient assessment should clearly describe the encounter, medical history, recent symptoms, and current functional status. Ongoing care plans outline treatment strategies, monitoring, and coordination of care between providers. Complete medication lists with any adjustments must be included. Counseling and patient education sessions require detailed notes about topics discussed.
Key documentation requirements include:
- Detailed patient assessment and care plan based on medical history, symptoms, and functional status
- Complete medication list with any dosage changes
- Counseling and education session notes covering discussed topics
- Care coordination with other providers like specialists and home health
- Any other patient encounters, assessments, or care plan updates
3). Time Spent on CCM Tasks
When submitting claims for Chronic Care Management (CCM) services to the CMS, it is vital to accurately document the time spent on each task. This is because reimbursement is directly tied to the time allocated per patient.
Healthcare providers must diligently maintain a record of the time spent on various CCM activities, such as:
☑️ ➜ Comprehensive patient assessment — Gathering and reviewing the patient’s medical history, current health status, and any potential risk factors.
☑️ ➜ Care plan development and implementation — Creating a personalized care plan tailored to the patient’s needs, addressing their chronic conditions, and ensuring its effective execution.
☑️ ➜ Medication management — Reviewing and optimizing the patient’s medication regimen, monitoring for potential interactions or side effects, and providing education on proper medication adherence.
☑️ ➜ Patient counseling and self-management education — Conducting counseling sessions to empower patients with the knowledge and skills necessary for self-care, including lifestyle modifications, disease management techniques, and preventive measures.
Additionally, healthcare providers should consider including the following relevant activities in their time documentation:
- Coordinating care with other healthcare professionals involved in the patient’s treatment plan.
- Providing 24/7 access to care management services for urgent or emergent needs.
- Facilitating transitions of care, such as hospital discharges or referrals to specialists.
- Conducting regular follow-up appointments or remote patient monitoring.
4). Billing Codes for CCM Services
Proper billing code assignment is needed for receiving reimbursement for chronic care management (CCM) services from CMS. By using specific CPT codes, practices can accurately report the CCM services provided and get paid for caring for patients with chronic conditions.
CCM services have designated CPT codes that should be used:
- 99490 – Chronic care management for patients with 2 or more chronic conditions
- 99439 – Chronic care management for patients with 1 or more chronic conditions
- 99487 – Complex chronic care management for patients with multiple comorbid conditions
- 99491 – Chronic care management for patients with 1 or more chronic conditions (first visit)
- 99489 – Chronic care management for patients with severe or complex conditions
- 99437 – Chronic care management for patients with 1 or more chronic conditions (subsequent visits)
Assigning the correct CPT code to CCM services is key for the following reasons:
- Ensures services are billed properly and practice receives appropriate reimbursement
- Allows payers like CMS to understand extent of non-face-to-face care coordination provided
- Demonstrates validity and medical necessity of billed CCM services
- Avoids claim denials or delays in payment due to incorrect coding
- Provides accurate data on services rendered for performance analysis and improvement
5). Claim Submission Frequency
Submitting claims for CCM services to the CMS also requires adherence to specific guidelines regarding claim submission frequency. Healthcare providers have the flexibility to submit CCM claims on a monthly, quarterly, or annual basis, depending on their preferences and the frequency of services provided to patients. It’s important to note that the claim submission frequency should align with the actual CCM services rendered to ensure accurate billing and reimbursement.
However, it’s crucial to remember that different insurance payers, including private insurers and Medicare Advantage plans, may have varying requirements regarding billing frequency for CCM services.
Therefore, healthcare providers should familiarize themselves with the specific guidelines set forth by each payer to ensure compliance and avoid potential claim denials or payment delays.
Key points to consider regarding CCM claim submission frequency:
👉 ➜ CCM claims can be submitted monthly, quarterly, or annually, aligning with the frequency of services provided.
👉 ➜ The claim submission frequency should accurately reflect the CCM services rendered to patients.
👉 ➜ Different insurance payers may have varying requirements for billing frequency, which healthcare providers must adhere to.
👉 ➜ Failure to comply with payer-specific guidelines can result in claim denials or payment delays.
👉 ➜ Regularly reviewing and updating billing practices based on payer guidelines is recommended to ensure compliance and timely reimbursement.
We’ll handle every detail, from time tracking to cost reports, to capture all the reimbursement you’ve earned.
Submitting Claims for CCM Services to CMS: A Step-by-Step Guide
As a healthcare provider offering Chronic Care Management (CCM) services, getting reimbursed from the Centers for Medicare & Medicaid Services (CMS) is important. However, the claims submission process can be daunting if you’re not well-prepared.
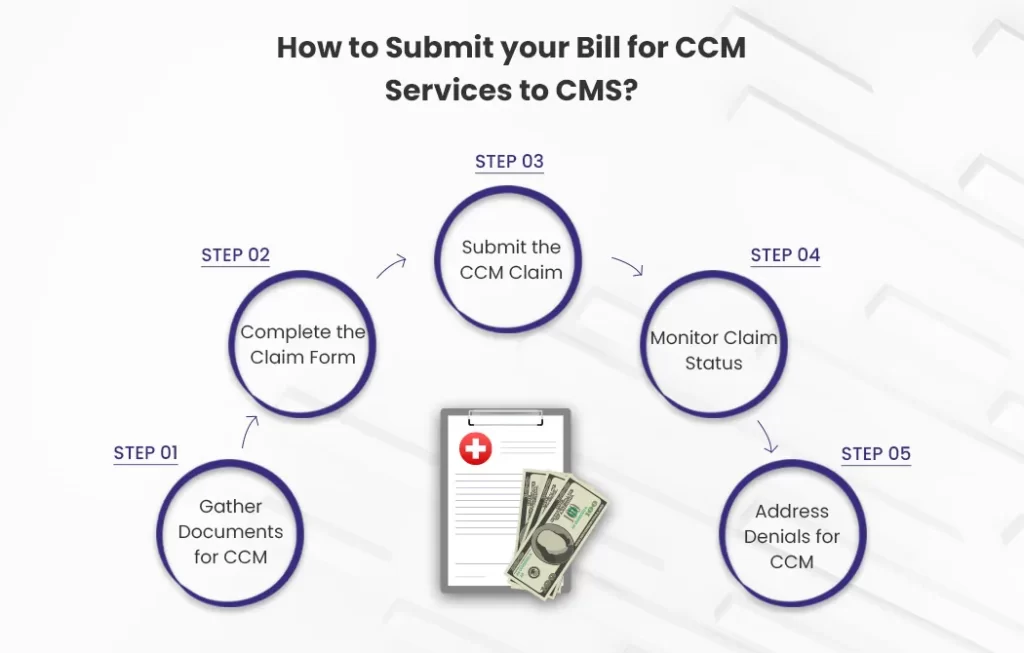
To ensure a smooth reimbursement process, follow these simple steps:
Step 1: Gather All Necessary Information
Before submitting your CCM claim, make sure you have all the required information at hand. This includes:
- Accurate CPT codes for the CCM services provided
- Detailed records of all CCM activities performed
- Complete patient demographics (name, date of birth, etc.)
- Patient’s insurance information (Medicare number, policy details, etc.)
Step 2: Choose the Right Claim Form
CMS accepts claims on the CMS-1500 form, which is specifically designed for professional services. Ensure that you fill out all fields accurately and completely to avoid any delays or denials.
Step 3: Submit Your Claim
The preferred method for submitting claims is through electronic means, such as a Certified Electronic Health Record Technology (CEHRT) or a clearinghouse. This streamlines the process and reduces the risk of errors. However, if electronic submission is not an option, you can still submit your claim via paper.
Step 4: Monitor Claim Status
After submitting your claim, it’s essential to monitor its status. You can do this by accessing the Medicare Provider Portal or contacting your insurance payer directly. This will help you stay on top of any issues or delays and take appropriate action if needed.
Step 5: Handle Claim Denials
If your claim is denied, don’t panic. Carefully review the reason for the denial and ensure that you have followed all the necessary guidelines. If you believe the denial was unjustified, you can resubmit your claim with additional supporting documentation or formally appeal the decision.
Remember, timely and accurate claims submission is key to receiving prompt reimbursement for your CCM services. By following these steps and staying organized, you can navigate the claims process with ease and ensure a steady revenue stream for your practice.
The Revenue Potential of Chronic Care Management (CCM)
Chronic Care Management (CCM) services offer a significant revenue opportunity for medical practices in 2024. With the latest Medicare reimbursement rate adjustments, CCM can become a valuable source of recurring revenue while improving patient outcomes.
The 2024 National Payment Rates for common CCM CPT codes are:
CPT 99490
- Non-facility: $61.56
- Facility: $48.79
CPT 99439
- Non-facility: $47.15
- Facility: $34.05
These rates are slightly lower than 2023, due to a 3.34% decrease in the Medicare conversion factor. However, CCM services remain profitable.

For example, let’s say a practice has 300 patients receiving CCM services per month. At the CPT 99491 reimbursement rate of $83 per patient, that’s $24,900 in monthly revenue from CCM alone.
On an annual basis, the revenue potential is even greater. With the same patient volume, annual CCM reimbursement would be $298,800. After paying a care manager’s salary of $50,000, the practice nets $248,800 in annual revenue just from CCM services.
The bottom line is that practices can generate significant revenue through Chronic Care Management in 2024, while also improving care coordination for their patients with chronic conditions.
CCM allows practices to be reimbursed for non-face-to-face care management services like:
- Regular patient check-ins and communication
- Medication management
- Care plan oversight and revision
- Care coordination with specialists
Making CCM a standard part of care delivery ensures patients get proactive support between office visits. This leads to better health outcomes and lower hospitalizations.
For any practice, focusing on CCM in 2024 is a smart financial move and an impactful way to elevate chronic care. The revenue potential is substantial, while the benefits for patients are even more meaningful.
FAQs
Is it possible CCM services can be billed for patients with only one chronic disease?
Yes, CCM services can absolutely be billed for patients with just one chronic condition. As long as that disease requires ongoing management and care coordination, you can bill CCM codes for those patients. The number of conditions doesn’t matter.
Can Chronic Care Management (CCM) be billed for telehealth visits?
Yes, you can bill CCM codes for telehealth services, as long as the platform used meets CMS guidelines and standards for telehealth. The telehealth medium itself does not impact CCM billing.
Can we bill more than one unit for CCM CPT code 99490 if we provide more than 20 minutes of CCM services?
No, only one unit of 99490 can be billed per patient per month. Even if you spend more than 20 minutes providing CCM services, you still can only bill for 1 unit. The threshold is 20 minutes per month.
What patient consent is needed to bill CCM codes?
Written consent is required before billing CCM codes. Patients must sign a document consenting to CCM services. Verbal consent alone is not enough. Make sure signed consent is on file.
How often can 99490 be billed? Is there a limit?
CPT code 99490 can be billed once per patient each calendar month. There is no annual limit on the number of times it can be reported as long as time requirements are met.
Can we bill 99490 if the patient is in a skilled nursing facility?
Unfortunately no. CCM services cannot be billed for patients who are in a skilled nursing facility, hospital, or similar institutional setting. The patient must be living at home.
What documentation is needed to bill CCM codes?
Thorough documentation of CCM services is required, including total time spent, care coordination activities, medication management, and creation of a care plan. Document everything in detail.
Do telehealth E/M services count toward the 99490 time requirement?
No. Time spent on E/M or telehealth visits cannot be counted toward the 20 minutes required for 99490. Only time spent on specific CCM activities can be included.
Can we bill 99490 if the patient only has 15 minutes of CCM services?
No, the threshold is 20 minutes per month. If the total time spent on CCM activities is less than 20 minutes, then 99490 cannot be billed. There are no exceptions for close calls.
How long should the care plan be for CCM billing?
There are no strict length requirements, but the care plan should thoroughly document the patient’s health issues, treatment goals, self-management, and coordination of care. Strive for 1-2 pages focusing on the patient’s chronic conditions.
Tapping into chronic care management revenue can be frustrating if you don’t have the right support. But BellMedEx makes it easy!
Our billing pros will ensure your documentation, time tracking, cost allocation, and claims submissions check every box. Let our CCM billing specialists do the heavy lifting while you focus on patient care.
CCM
‘Billing
help is here 🌌