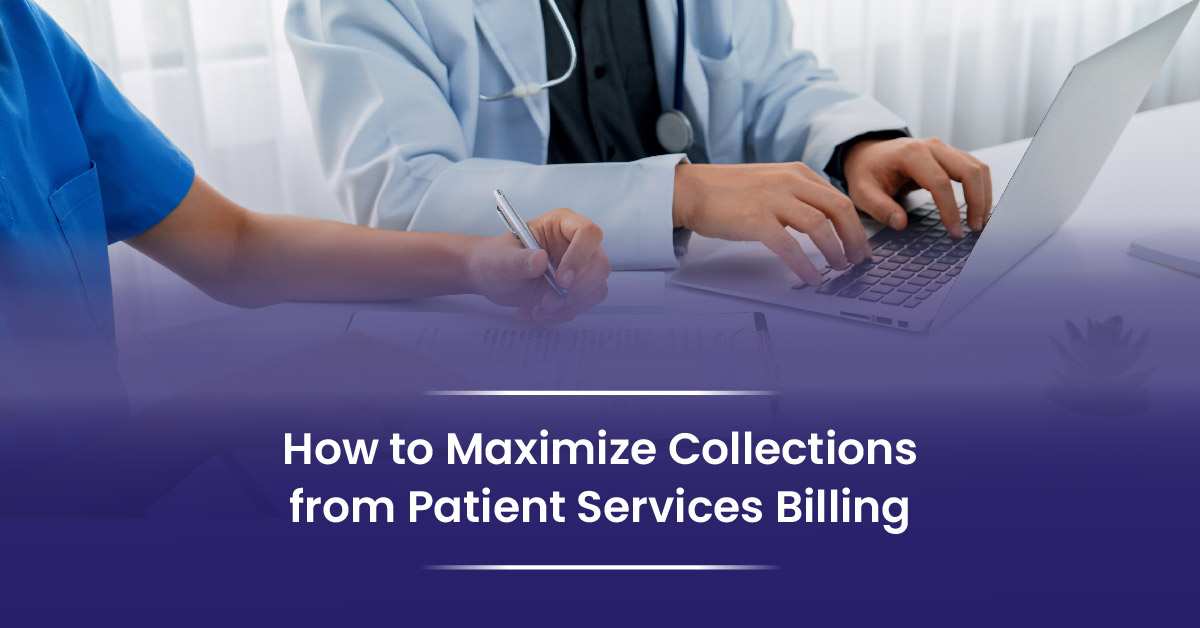
Studies show that up to 30% of medical revenue is lost due to billing errors and delays.
That’s a big hit to any practice. Maximizing collections from patient services billing helps close that gap and keeps your clinic financially strong.
In this guide, you’ll learn how to improve your billing process, collect payments more efficiently, and support long-term success in your healthcare setting.
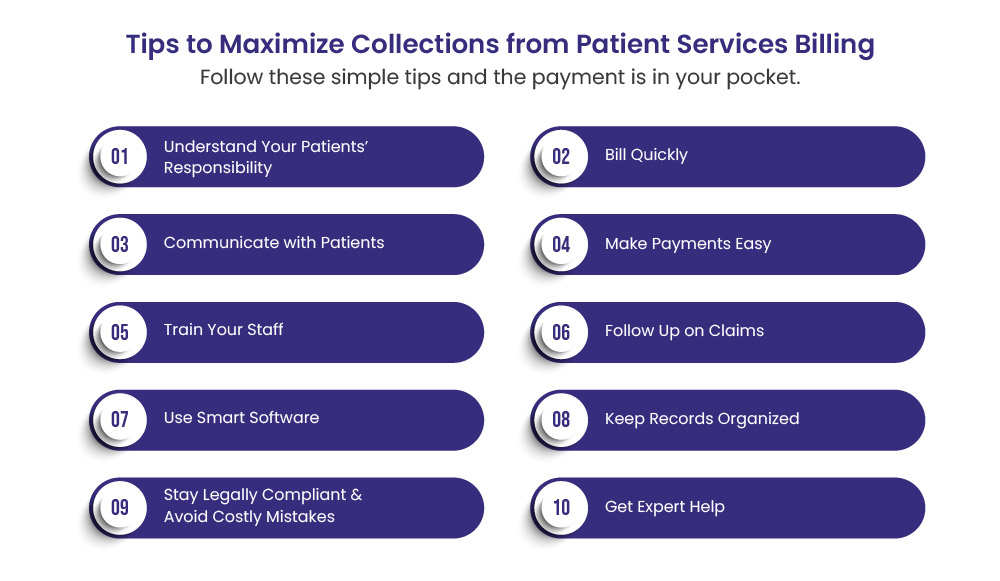
Step #1: Understand Your Patients’ Responsibility
Before you ask a patient to pay, make sure the bill is right. Healthcare providers lose money because of small mistakes. These include wrong charges, missing details, or unclear bills. A clean and accurate bill helps patients understand what they owe and makes it easier for them to pay.
Here’s how to make sure your patient billing is on point:
Use correct service codes
Match each code to the care provided. This keeps the bill clear and fair.
Check patient details
Confirm names, contact info, and coverage before billing. Mistakes here can cause confusion or delays.
Review charges carefully
Make sure all services are listed and priced correctly. Don’t leave anything out.
Give a clear summary
Share a simple breakdown of costs with the patient. Use plain language and avoid jargon.
Tip: Keep a billing checklist at your front desk or billing station. It helps your team stay sharp and avoid costly mistakes.
Step #2: Bill Quickly
Speed matters in medical billing. The longer you wait to send a claim, the harder it becomes to collect. Delays can lead to missed deadlines, denied claims, or even forgotten charges. Fast billing shows that your practice is organized and serious about getting paid.
Here’s how to keep billing fast and smooth:
Submit claims within 24–48 hours
Don’t let paperwork sit. Make billing part of your daily routine.
Use medical billing software
Good tools help you fill forms fast, catch missing info, and send claims with a click.
Set clear roles
Assign billing tasks to specific staff. Everyone should know who handles what. But, I would suggest outsourcing it.
Avoid batching
Don’t wait to send claims in bulk. Send them as soon as each patient visit is done.
Tip: Create a simple billing calendar or checklist. It helps your team stay on track and avoid delays.
Step #3. Communicate with Patients
Perfect billing starts with good communication. Patients are more likely to pay when they understand what they owe and why. Send them bills with clear details. Many billing issues come from confusion, not refusal. A clear, kind message can make all the difference.
Here’s how to talk about billing in a helpful way:
Explain costs early
Share fee details before or during the visit. Don’t surprise patients later.
Use simple words
Avoid medical or billing jargon. Keep it short and clear.
Give written info
Hand out printed bills or email a summary. Let patients review it in their own time.
Be open to questions
Make space for patients to ask. Listen and respond with care.
Stay polite but firm
Be kind, but don’t avoid the topic. Clear rules help everyone.
Step #4. Make Payments Easy
Even when patients want to pay, the process can feel hard. Long forms, limited options, or confusing steps can slow things down. If you make it easy, you’ll get paid faster and more often.
Here’s how to simplify payments for your patients:
Offer multiple payment options
Accept credit cards, mobile wallets, and online payments. Let patients choose what works best.
Set up payment plans
For large bills, break the total into smaller monthly payments. This makes it less stressful for patients.
Send reminders
Use text messages or emails to remind patients about upcoming or missed payments.
Use a patient portal
A secure online portal lets patients view bills, ask questions, and pay anytime.
Tip: The easier it is to pay, the fewer excuses you’ll hear. Convenience leads to better collections.
Step #5. Train Your Staff
Your billing system is only as strong as the people who run it. Even the best software won’t help if your team doesn’t know how to use it well. Training your staff helps reduce mistakes, speed up billing, and improve collections.
Here’s how to build a strong billing team:
Teach billing basics
Make sure your staff knows how to enter codes, check insurance, and follow billing rules.
Hold regular training
Set up short monthly sessions to review updates, common errors, and best practices.
Use real examples
Show your team how to fix denied claims or spot missing info using actual cases.
Encourage questions
Create a space where staff can ask and learn without fear. It builds confidence and skill.
Assign clear roles
Your staff should know who handles billing, follow-ups, and patient questions.
Step #6. Follow Up on Submitted Claims to the Insurer
Sending a claim is just the start. Many claims get stuck, denied, or ignored. If you don’t follow up, you may never get paid. Staying on top of your claims helps you catch problems early and fix them fast.
Here’s how to stay in control of your billing:
Track every claim
Use automated software to see which claims are paid, pending, or denied.
Act fast on denials
Don’t wait. Review the reason, fix the issue, and resubmit quickly.
Call payers when needed
If a claim is stuck, pick up the phone. A short call can solve a long delay.
Keep notes
Write down who you spoke to, what they said, and what steps you took.
Set reminders
Use alerts or calendars to follow up on claims that haven’t moved.
Tip: The longer a claim sits, the harder it is to collect. A quick follow-up can save weeks of waiting.
Step #7. Use Smart Software
Billing by hand takes time and leads to errors. Smart software can speed things up, catch mistakes, and help you get paid faster. It also keeps your data safe and your team organized.
Here’s how to choose and use the right tools:
Pick software that fits your clinic
Small practices need simple tools. Big clinics may need more features. Choose what works for your size. However, I would suggest going for BellMedEx advanced software for best billing practices.
Look for auto-coding and alerts
These features help you bill faster and avoid common errors.
Use dashboards and reports
See which claims are paid, pending, or denied—all in one place.
Make sure it’s secure
Patient data must be protected according to HIPAA rules. Choose software with strong privacy settings.
Train your team to use it well
Even the best tool won’t help if no one knows how to use it. We can offer you free training once you partner with BellMedEx.
Tip: A good billing system pays for itself. It saves time, reduces stress, and helps you collect more.
Step #8. Keep Records Organized
Good records are the backbone of strong billing. When files are messy or hard to find, it slows everything down. Clean records help you fix problems fast, follow up on claims, and stay ready for audits.
Here’s how to keep your billing records in shape:
Use clear names and dates
Label files so anyone can find them quickly. Avoid vague names like “doc1” or “misc.”
Sort by type
Group files by patient, service date, or claim status. Use folders or tags to stay organized.
Keep notes on changes
If you update a bill or speak with a payer, write it down. These notes help if issues come up later.
Back up your data
Use secure cloud storage or external drives. Don’t risk losing key info.
Review records often
Set time each week to clean up old files and check for missing details.
Step #9. Stay Legally Compliant & Avoid Costly Mistakes
While speed, accuracy, and communication are essential for effective billing, compliance with healthcare regulations is equally critical. Ignoring legal requirements can result in denied claims, audits, heavy fines, or even criminal penalties for fraud or abuse.
Know the Rules
You don’t need to be a lawyer, but your team should know the basics of healthcare billing laws:
HIPAA
Protect your patients’ private information. That means using secure software, locking your screens, and keeping patient files safe.
False Claims Act
Don’t bill for something you didn’t do or for more than you did. Even small mistakes can lead to big problems.
Upcoding and unbundling
These are billing errors that happen when you use the wrong codes to get paid more. Always bill honestly and correctly.
Stark Law and Anti-Kickback Rules
Don’t refer patients or accept referrals based on gifts or deals. Keep your referrals clean and based on care, not money.
Watch Out for These Mistakes
Some billing errors are more than just a mistake—they can be seen as fraud. Avoid these common issues:
- Billing for services that weren’t done
- Using the wrong code to get paid more
- Splitting up codes that should be grouped
- Charging the same thing twice
- Billing without medical notes to back it up
Tip: A little effort now saves big trouble later. Staying compliant protects your practice and your patients
Step #10: Get Expert Help from Medical Billing Specialists
Sometimes, even with the best team and tools, billing can still feel tough. Rules change, claims get denied, and time runs short. That’s when expert help can make a big difference. Bringing in a medical billing expert can boost your collections and free up your staff to focus on care.
Here’s how to make expert support work for you:
Hire a billing consultant or firm
Choose someone with healthcare experience. They know the rules and can spot issues fast.
Check reviews and references
Ask other clinics who they trust. Look for proven results and good service.
Set clear goals
Tell your billing partner what you expect: faster claims, fewer denials, better tracking.
Stay involved
Don’t hand off everything. Keep checking reports and asking questions.
Use them for training too
Experts can teach your team and help improve your in-house process.
FAQs
What should we do if a patient refuses to pay their bill?
Start with a kind follow-up message. If they still don’t pay, offer a payment plan or ask why they’re not paying. If needed, you can send the account to collections, but only after trying everything else first.
Can we charge a fee for late payments?
Yes, but only if your policy is clear and shared with the patient up front. Always include it in your financial policy form and have the patient sign it.
Should we verify insurance before every visit, even for returning patients?
Yes. Insurance plans can change at any time. Always check before each visit to avoid denied claims or billing the wrong payer.
Is it okay to bill a patient before insurance pays?
It’s better to wait for the insurance response first. Once the insurance has paid its part, you can send the patient a bill for the remaining balance.
Do we need patient consent to send electronic bills or reminders?
Yes. Always get permission before sending text messages or emails about billing. Add a consent form during registration or in the patient portal.