Medical billing is a complex process. Practices must ensure efficiency and accuracy in the whole process. This will help them to get reimbursed by insurance providers successfully, and there will be an increase in cash flow and patient satisfaction. However, there are chances of mistakes in the billing process that must be addressed accordingly. In this blog post, we will discuss some common mistakes in medical billing, their consequences, and some actionable tips to avoid them.
Common Medical Billing Mistakes
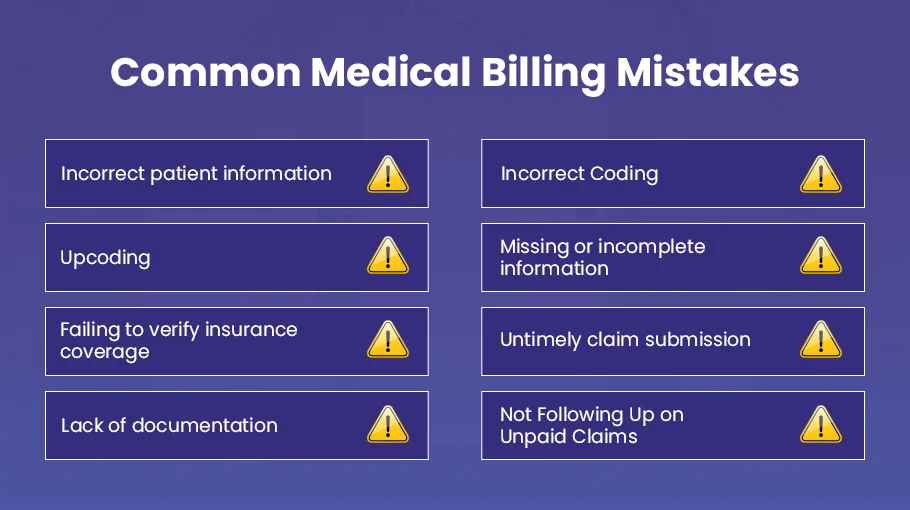
Let’s discuss the common medical billing mistakes in detail
Incorrect patient information
Ensuring accurate and up-to-date patient information is vital in the healthcare industry. Incorrect patient information can lead to claim denials or delays in payment. For instance, a small typo in the patient’s address can result in an insurance claim being returned as undeliverable, leading to delayed payments or even denied claims.
Incorrect Coding
Correct diagnosis and procedure codes and modifiers are essential for accurate billing. Errors in code assignment can lead to claim denials and delays in payment.
Upcoding
Accurately assigning codes to services is necessary to avoid upcoding for services. Upcoding can lead to audits, fines, or claim denials.
Missing or incomplete information
Submitting complete and accurate information for all fields in a claim, including provider information, patient demographics, and insurance details, is necessary. Missing or incomplete information can lead to claim denials or delays in payment, causing additional work and time for healthcare providers.
Failing to verify insurance coverage
Before submitting a claim, healthcare providers must verify the patient’s insurance coverage, including eligibility, benefits, and preauthorization requirements. Failing to do so can result in claim denials or delays in payment, causing financial losses to the medical practice and frustration for the patient.
Untimely claim submission
Submitting claims within the payer’s specified timeframe is necessary to avoid claim denials or delays in payment. Timely submission can lead to quicker payments and better cash flow for the medical practice.
Lack of documentation
Thorough and accurate documentation is necessary to support the services billed. This is essential for claim approval and to avoid potential audits. Healthcare providers must ensure that all relevant documents are included with the claim.
Not Following Up on Unpaid Claims
Failure to follow up on unpaid claims is a common mistake in medical billing. After submitting claims, it’s essential to monitor and follow up on unpaid claims regularly. Unpaid claims can result in lost revenue and delayed payment for services provided.
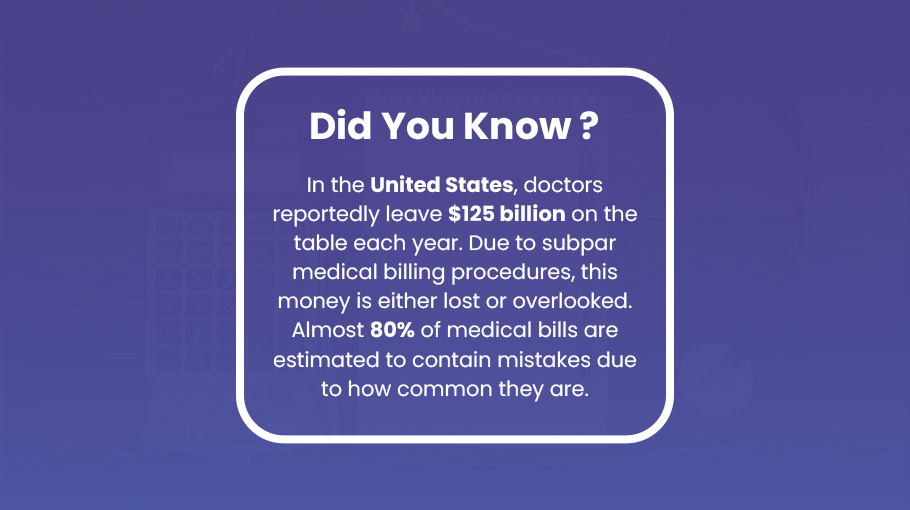
Impact of Medical Billing Mistakes on Healthcare Providers
Medical billing plays a vital role in the healthcare industry. Accurate and efficient billing is necessary for healthcare providers to receive timely and appropriate service reimbursement. However, medical billing errors can significantly impact healthcare providers and patients.
Here’s a closer look at the impact of medical billing on healthcare providers:
Financial Impact
Medical billing errors can have a significant financial impact on healthcare providers. When claims are denied, delayed, or rejected, healthcare providers may experience cash flow issues, affecting their ability to pay for overhead expenses such as rent, salaries, and supplies. This can also lead to cutbacks in staffing or services, further impacting the quality of patient care.
Administrative Burden
Medical billing requires extensive administrative work, including submitting claims, following up on denials, and resubmitting claims. When errors occur, additional administrative work is necessary to correct the errors and resubmit the claims. This can increase healthcare providers’ administrative burden, taking away valuable time and resources from patient care.
Legal and Compliance Issues
Medical billing errors can result in legal and compliance issues like HIPAA Compliance for healthcare providers. These issues can include audits, fines, and even lawsuits. Healthcare providers must comply with numerous regulations and guidelines related to medical billing and coding, and any errors can result in noncompliance and legal consequences.
Reputation
Medical billing errors can also impact the reputation of healthcare providers. Patients who receive unexpected bills due to billing errors may become frustrated and lose trust in their healthcare providers. Negative reviews and decreased referrals can also damage the reputation of healthcare providers.
Increased administrative costs
When billing errors occur, additional administrative work is required to correct the errors and resubmit claims. This can lead to increased administrative costs for healthcare providers, including extra staff time, software expenses, and other resources. These costs can add up quickly and impact the financial stability of healthcare practices, especially for smaller practices with limited resources. In addition, increased administrative costs can divert resources away from other essential patient care areas, impacting the overall quality of care.
How to Avoid Common Medical Billing Mistakes
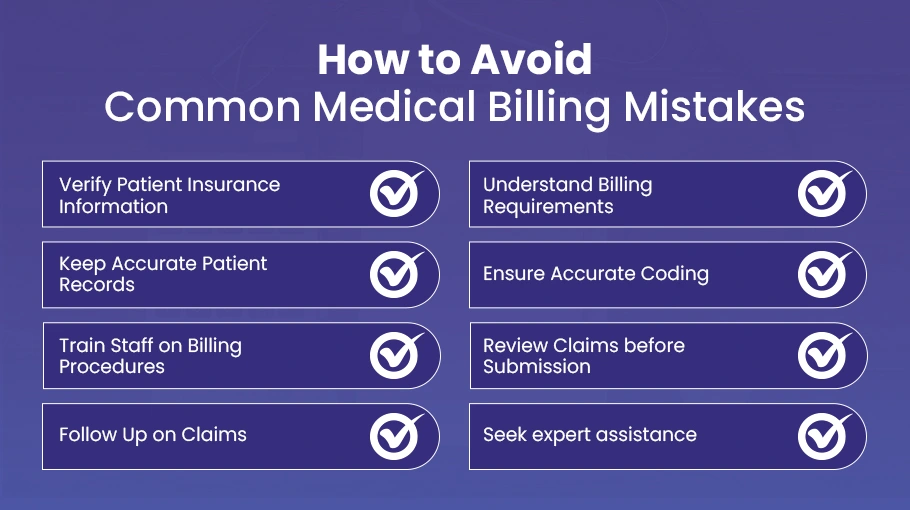
Medical billing mistakes can cause significant financial losses and inconvenience healthcare providers and patients. Here are some pro tips for healthcare providers to avoid medical billing mistakes:
Verify Patient Insurance Information
Verifying the patient’s insurance information before providing any services is essential. Providers should check whether the patient’s insurance policy is active, what services are covered, and if there are any limitations or exclusions.
Understand Billing Requirements
Providers must be familiar with different insurance companies’ coding and billing requirements. Familiarity with these requirements can help providers avoid common medical billing mistakes resulting in claim denials or delays.
Keep Accurate Patient Records
Providers should maintain accurate and up-to-date patient records, including medical history, medication lists, and insurance information. Accurate patient records can help providers avoid medical billing mistakes and ensure they provide the correct services.
Ensure Accurate Coding
Coding errors can lead to denied claims, delayed payments, or underpayment for services provided. To avoid coding mistakes, train qualified staff to handle medical coding. You can also use Electronic Health Records (EHR) to streamline the coding process and reduce the risk of errors.
Train Staff on Billing Procedures
Training all staff on billing procedures is essential to ensure everyone follows the same process. This training can help prevent billing errors, identify potential issues before they become problems, and ensure everyone follows best practices.
Review Claims before Submission
Providers should review all claims before submitting them to ensure they are accurate and complete. Reviewing claims can help providers catch errors before they are submitted and avoid delays in reimbursement.
Follow Up on Claims
Providers must follow up on all the claims they submit to verify that they are being processed accurately. This follow-up process can assist providers in identifying and resolving any potential issues before they escalate into more significant problems.
Seek Expert Assistance
Providers should seek expert assistance from medical billing companies like Bell MedEx if they are unsure about coding, billing, or insurance requirements. These experts can help providers navigate complex billing processes and avoid common mistakes.
By implementing these tips, healthcare providers can avoid common medical billing mistakes and ensure they provide high-quality patient care.
Conclusion
Avoiding common mistakes in medical billing is crucial to avoid denied claims, delayed payments, and lost revenue. By sidestepping the pitfalls discussed in this article, you can streamline your revenue cycle management and improve your bottom line. Ensuring proper documentation, accurate coding, correct patient information, verified insurance coverage, and establishing a system to follow up on unpaid claims are essential to avoid these common mistakes and enhance your medical billing process.
You can boost revenue, minimize errors, and provide better patient care with the right approach and systems. Therefore, taking the necessary steps to avoid these errors and improve your medical billing process is vital.