In the world of healthcare billing, two key terms often come up: institutional claims and professional claims. Now, some bills are for the doctor’s service (professional), while others are for the hospital itself (institutional) explaining who’s charging for what – the doctor or the hospital.
Knowing the difference between these two is crucial for both healthcare providers to be aware of what they should be paid and for patients to understand their bills. This article will uncover what each type of claim entails, why it’s important to understand the distinction, and how to navigate these confusing bills to ensure your practice is getting paid properly.
What are Institutional Claims (837-I)?
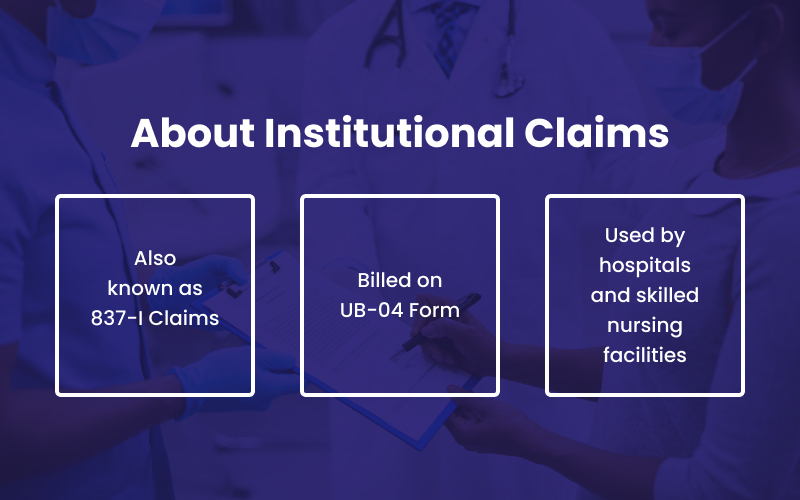
Institutional claims also known as 837 I claims (I for institutional format) are submitted to insurance companies by hospitals and skilled nursing facilities for in-patient and out-patient services performed. For this reason, hospital billing is often known as institutional billing.
These claims are billed on a UB-04 form, previously known as the CMS-1450 form. It bills claims for medical services such as laboratory tests, medical supplies, equipment, imaging, etc, and for the use of the healthcare facility itself, like hospitals, nursing homes, or specialized clinics.
Institutional claims come from hospitals or SNF therefore, hospital doctors and the medical professionals performing their services will need the UB-04 institutional form.
➤ Types of Institutional Claims
The three main types of institutional billing claims are:
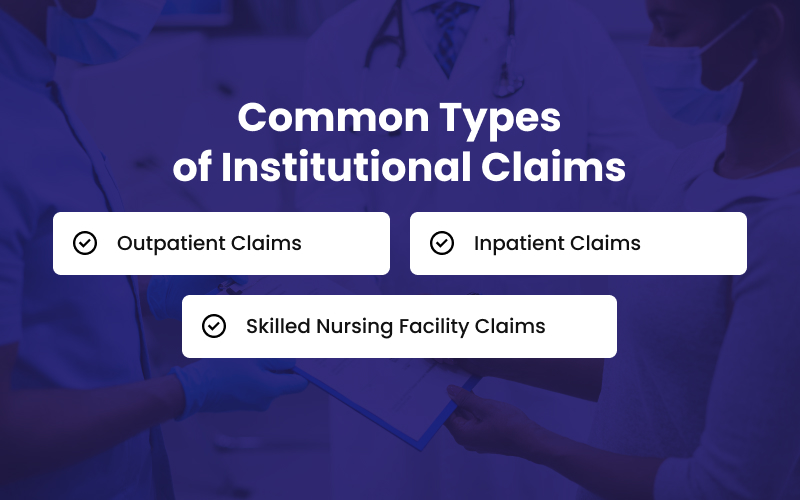
Outpatient Claims
These are the claims generated by physicians who treat patients at their clinic, for example, visit with healthcare providers such as dentists, eye care doctors, or mental health professionals.
Inpatient Claims
The claims generated for the patients who stay in the hospital and use the facility are inpatient claims. For example, tests, procedures, surgeries, room charges for overnight stays in hospital wings or intensive care units (ICUs), nursing care, prescriptions, and medical supplies.
Skilled Nursing Facility Claims
These types of institutional claims are generated by the skilled nursing homes for patients that need long-term care. For example, the specialized care and facilities provided to the patients who need rehabilitation and extended medical attention.
➤ Purpose of Submitting Institutional Claims
Since institutional claims involve multiple services and providers, these are more complex and therefore, need to be accurately documented and coded. These claims are made on specified forms and the purpose of filing an institutional claim is to get reimbursed for the services delivered by the hospital or clinic.
➤ Common Challenges Faced In Institutional Claims
Institutional challenges include confusion over;
- Revenue codes
- Complicated software
- Medicare denials
- Resource limitations
- System consolidation issues.
Using a comprehensive approach such as best outsourced medical billing services, advanced technology, and an expert team of billers and coders saves you from denials and losing reimbursements.
What are Professional Claims (837-P)?
Professional claims are generated by physicians, nurses, suppliers, and other medical staff for both outpatient and inpatient services. These charges are billed on a CMS-1500 form, whose electronic version is called 837- P (P for Professional format).
For example; routine office visits and laboratory services.
➤ Types of Professional Claims
The three main types of professional claims are:
Physician Claims
Physician billing claims include diagnostic and treatment services provided by licensed doctors. These claims are submitted by various specialties such as cardiologists, general practitioners, surgeons, pediatricians, etc to ensure reimbursement for the professional services delivered.
Consultations and Specialist Visit Claims:
Not just treatments but consultations with specialists are also covered by professional claims. Specialist consultations be it neurologists, pediatricians, dermatologists or any other specialist, bill their services using professional claims.
Emergency Department Claims
The care delivered to the patients by the emergency department such as physicians, nurses, and other staff is billed through professional claims.
➤ Purpose of Submitting Professional Claims
The purpose of submitting all and especially professional claims is to ensure that a healthcare practice is reimbursed for the services rendered by its healthcare professionals such as nurses and physicians. The accurate documentation of codes helps create claims that are submitted to insurance companies or other third-party payers for payment.
➤ Common Challenges Faced In Professional Billing Claims
Entities bound to use professional claims for reimbursement, may face challenges like;
- Staff shortages
- Payer changes
- Coding complexity
- Claim denials
- Patient responsibility
The accurate documentation of codes for various services delivered, improved front-end processes, and prioritized payer relationships help you optimize your professional claims and overall billing operations while enhancing overall financial growth.
Key Differences Between Institutional and Professional Claims
| Feature | Institutional Claim | Professional Claim |
| Billing Entities | Hospitals | Individual Practitioners |
| Form Used | UB-04 Form | CMS-1500 Form |
| Types of Services | ◉ Inpatient ◉ Outpatient ◉ Skilled Nursing Facility |
◉ Physician Claims ◉ Consultations and Specialist Visit ◉ Emergency Department Claims |
| Coding Systems | ◉ HCPCS (Healthcare Common Procedure Coding System) ◉ DRGs (Diagnosis-Related Groups) |
◉ CPT (Current Procedural Terminology) ◉ ICD-10 (International Classification of Diseases, 10th Revision) |
| Reimbursement Rates | ◉ Case rates ◉ DRGs ◉ Daily charges ◉ Bundled payments, or other combined payment schemes |
Fee-for-Service with CPT codes |
| Impact on Revenue Generation | Higher revenue due to facility-based care | Lower revenue due to less expensive outpatient care |
Accurately Submit Institutional and Professional Claims With BellMedEx
It can get difficult for your medical staff to keep a balance between two different tasks such as providing care and submitting billing claims. It requires a completely unique set of skills, expertise, time, and effort to manage both aspects of a healthcare practice. You see, managing the two tasks together can affect the overall productivity of your staff as well as the patient experience.
This is where BellMedEx, a medical claims billing service company comes in. Our medical billers and coders are certified by the American Medical Association (AMA), American Academy of Professional Coders (AAPC), and Certified Professional Billers (CPB) and are well-trained to create the right codes and generate accurate claims.
We handle professional and institutional medical claims for both small medical practices and large healthcare facilities. Our professionals stay updated with the latest institutional and professional claim submission standards which means your claims will always be compliant and quickly reimbursed without being denied or delayed.
Click here to schedule a free medical billing consultancy regarding claim submission or contact us directly at 888-987-6250.