Medical billing services connect healthcare providers and payers, essential for revenue cycle management. They translate healthcare services into codes, submit claims, follow up with insurance companies, and get providers paid.
But the question is: what is the standard fee for a medical billing service?
The cost of medical billing services varies depending on the practice size, services provided, and the billing company’s pricing model.
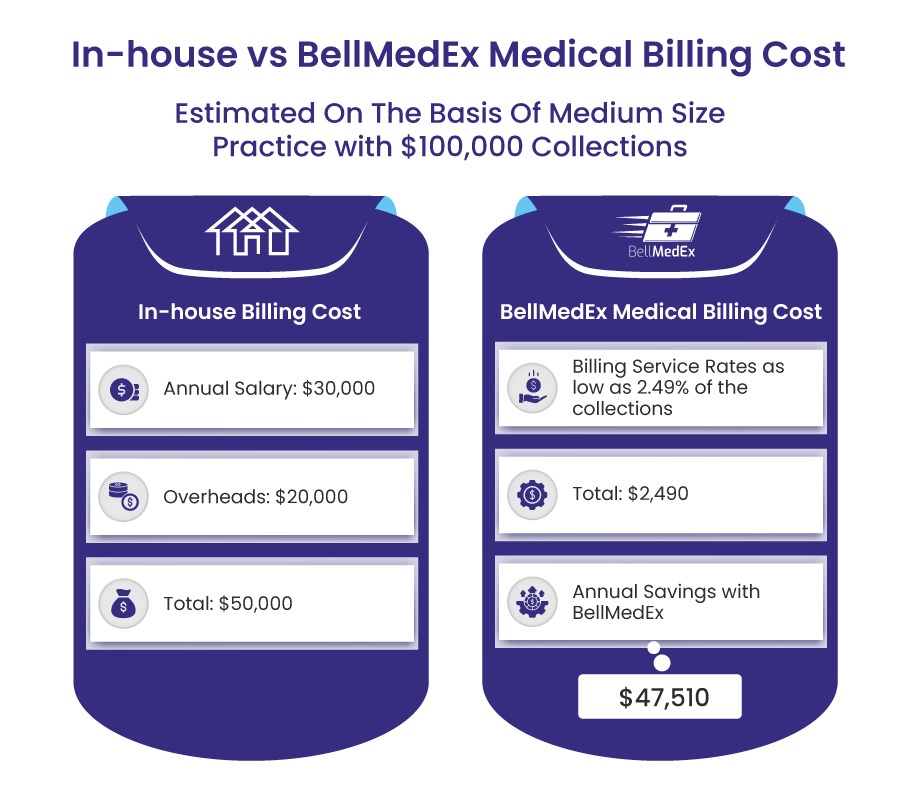
If you are confused about your decision whether to outsource medical billing services or go for in-house billing .You need to be clear that outsourcing medical billing services is a cost effective option for your healthcare practice rather than managing it in-house. Before getting into the pricing models, here’s an estimate of cost based on medium sized practice with $100,000 collections.
Therefore, healthcare providers should be aware of pricing structures and individual requirements to make informed decisions.
What Factors Determine Medical Billing Rates?
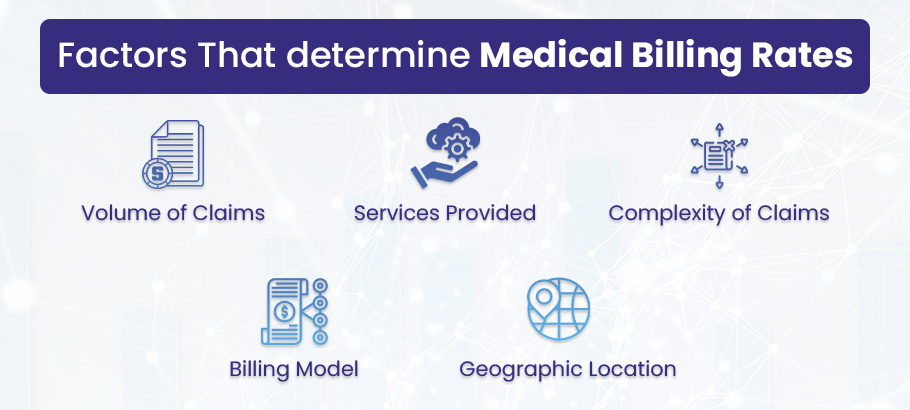
The following are some of the factors that determine medical billing rates. You need to know these in order to estimate the cost of medical billing services:
Volume of Claims. A larger volume of claims generally requires more work and thus results in higher fees.
Services Provided. The cost of services can vary depending on the type and scope of services provided. Comprehensive services, such as patient registration, insurance verification, coding, billing, and collections, typically cost more than claim submission services.
Complexity of Claims. Practices with complex claims that require extensive coding or special handling might pay higher fees.
Billing Model. Billing companies may charge a percentage of the amount collected, a flat fee per claim, or an hourly rate. The best model depends on the practice’s claim volume, average claim value, and other factors.
Geographic Location. Medical billing service rates might also differ by region owing to variations in the cost of living and market competition.
Understanding Medical Billing Charges
Medical billing charges can be classified into two categories: transactional and administrative fees.
Transactional fees are expenses that come with submitting and processing claims. This includes costs for electronically submitting a claim, posting payments, handling patient statements, and managing denied or rejected claims. These fees are often variable, meaning they can change depending on the volume and complexity of claims made.
Administrative fees are the costs involved in overseeing the billing process. This includes patient registration, insurance verification, appointment scheduling, and account management. Unlike transactional fees, administrative fees are often fixed. However, they can also fluctuate depending on the size of the healthcare provider and the complexity of their services.
In addition, many medical billing companies charge an initial setup fee. This fee covers the costs of integrating their system with the healthcare provider’s electronic medical records (EMR) system, training the staff, and establishing the necessary workflows. The amount of these fees can vary, often becoming quite substantial for larger practices with more complex needs.
By managing all these costs BellMedEx helps you to increase revenue upto 30%.
Medical Billing Service Pricing Structures
While rates can vary widely depending on different factors like the size of the medical practice, providers can generally expect to pay:
- 4% to 9% of collected revenue for full-service medical billing under a percentage-based model.
- $4 to $7 per claim under a flat fee model.
- $20 to $30 per hour under an hourly fee model.
It’s important to note that these are rough approximations, and actual costs may be higher or lower depending on the specific circumstances of the healthcare practice.
BellMedEx is your partner to provide cost effective solutions that help your healthcare practice to save revenue up to 30%. Get a complete demo how we are your helping hands in all your medical billing process.
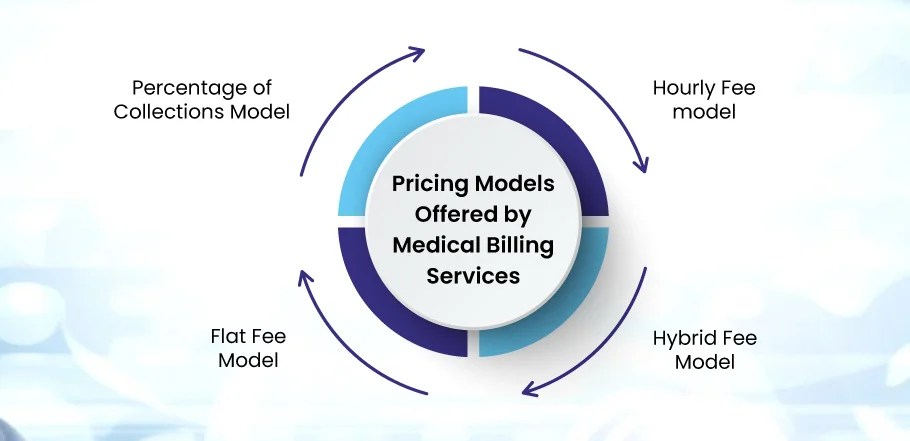
Medical Billing Services Pricing Models
Percentage of Collections Model
In this model, billing services are paid a percentage of the total collections they handle for the healthcare provider. This percentage can range from 4% to 10% and usually depends on the volume and complexity of the billing tasks. This model can motivate billing services to increase collections, as their payment is tied to the provider’s earnings. However, it can potentially be more expensive if collections are high.
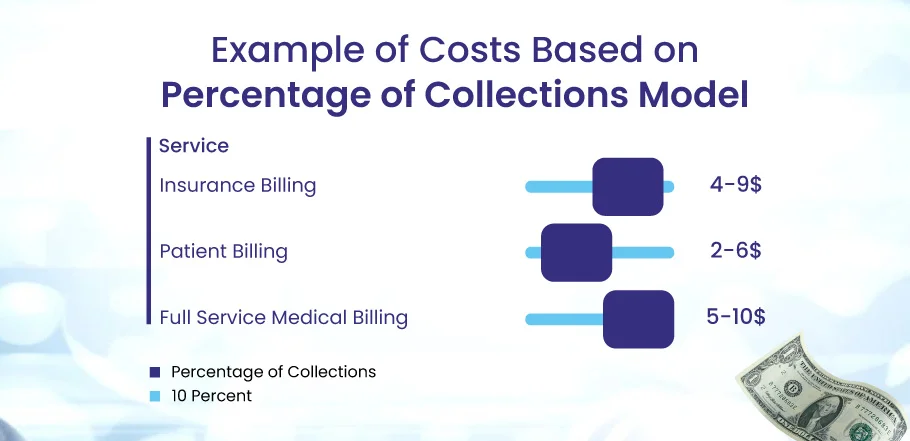
This image shows the costs for different services based on a percentage of the collections model:
- For insurance billing, the service provider charges between 4% to 9% of the collections.
- For patient billing, the service provider charges between 2% to 6% of the collections.
- For full-service billing, the service provider charges between 5% to 10% of the collections.
| Pros | Cons |
| ✅ Aligns the billing service’s incentives with those of the provider. | ❌ Can be more expensive if collections are high. |
| ✅ Flexible concerning the volume and complexity of claims. | ❌ May incentivize billing services to focus on higher-value claims. |
Flat Fee Model
In this model, a set price is charged per claim or patient encounter. This usually covers all billing stages, from claim submission to payment posting and tracking of any follow-ups. While the flat fee model provides cost certainty, it might not always reflect the time and effort needed for handling complex or challenging claims.
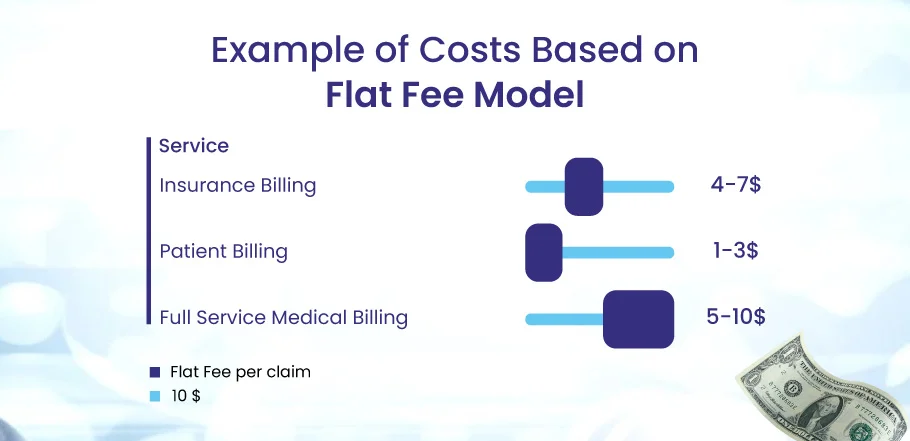
This image shows the costs for different services based on a flat fee-per-claim model:
- For insurance billing, the service provider charges between $4 to $7 per claim.
- For patient billing, the service provider charges between $1 to $3 per claim.
- For full-service billing, the service provider charges between $5 to $10 per claim.
| Pros | Cons |
| ✅ Predictable costs | ❌ It may not accurately reflect the effort and time for complex or problematic claims. |
| ✅ Simplicity in understanding and managing costs | ❌ The flat fee may not cover unexpected complications or tasks. |
Hourly Fee Model
In this model, a fee is charged for each hour spent on billing tasks. This provides a clear breakdown of costs, ensuring that the client only pays for the work that is done. However, the amount of time required can vary greatly, making it difficult to estimate costs upfront.
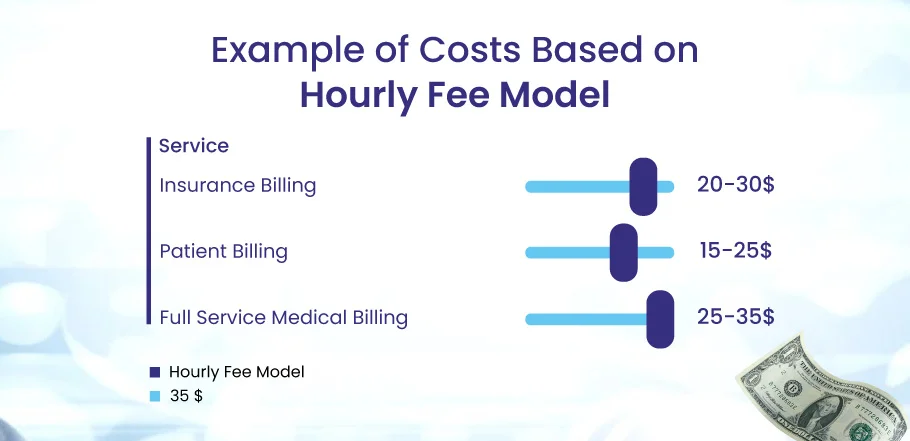
This image shows the costs for different services based on an hourly fee model:
- For insurance billing, the service provider charges $20 to $30 per hour.
- For patient billing, the service provider charges $15 to 25 per hour.
- For full-service billing, the service provider charges $25 to $35 per hour.
| Pros | Cons |
| ✅ Provides a clear breakdown of where costs are incurred. | ❌ Difficult to predict costs due to variability in time required. |
| ✅ Ensures the provider pays only for actual work done. | ❌ May incentivize slower work to increase billable hours. |
Hybrid Fee Model
This model combines the other pricing structures, such as the Percentage of Collections Model and the Flat fee model. A flat fee may be charged for claim submission, with an additional percentage from successful collections. This model is tailored to the specific needs of the provider, offering flexibility. However, it may be more complex to manage than the other models.
| Pros | Cons |
| ✅ It offers flexibility and can be tailored to specific needs. | ❌ It can be more complex to manage and understand due to the combination of pricing structures. |
| ✅ Balances predictable costs (flat fee) with incentivized success (percentage of collections). | ❌ It can become more expensive, depending on the balance of flat and percentage fees |
Other Types of Fees
Other types of medical billing fees include clearinghouse fees, monthly minimum fees, and hidden fees.
Clearinghouse Fees
Clearinghouse fees are charges associated with checking and transmitting medical claims to payers. Clearinghouses ensure that claims are accurate and compliant with payer requirements before submission. Fees can be charged per claim or as a flat monthly fee, ranging from a few cents to several dollars per claim.
Monthly Minimums
Some billing services impose a monthly minimum fee. This can be a flat fee or a minimum percentage of collections. If a provider’s claim volume or collections are low, this can effectively increase the per-claim cost. Providers should be aware of any monthly minimums when evaluating a billing service.
Hidden Fees
Hidden fees can include charges for services that are not included in the base price, such as patient statements, claim resubmissions, data backups, or software upgrades. Providers should carefully review their contracts to ensure they understand all potential charges.
Healthcare Software Pricing for Medical Services Providers
The pricing of healthcare software is typically based on the number of users, the complexity of the features, and the deployment method (cloud-based or on-premises). Some software providers offer a suite of integrated products, with each module or feature having an additional cost. There is often an initial setup or implementation cost, followed by a regular subscription fee for continued use and support.
The common pricing models of healthcare softwares are:
Subscription is a pricing model in which customers pay a regular fee (monthly or yearly) to access software. The price is often based on the number of users or the amount of usage. Subscription fees typically cover customer support, updates, and maintenance.
Perpetual is a pricing model in which the user pays a one-time fee to own the software for an unlimited period of time. However, there may be additional costs for maintenance, support, and updates.
Freemium is a pricing model that gives users access to basic features for free while charging for additional features or capabilities. This allows users to try the software before they buy it.
| Plan | Cost |
| Basic EHR | Free |
| Pro EHR | 35/provider/month |
| Ultimate EHR+PMS | $49/provider/month |
| RCM | Starting at 2.99% |
| Enterprise for Larger Groups | $49 |
Value-based reimbursement in healthcare is an alternative to the traditional fee-for-service model. Rather than paying for each service or test provided, value-based reimbursement ties payments to the quality of care delivered. This approach encourages providers to focus on providing effective and efficient care that results in better health outcomes for patients.
The value-based billing model is becoming more popular. The Centers for Medicare & Medicaid Services (CMS) has launched several value-based care models, such as the Medicare Shared Savings Program, the Next Generation ACO Model, and the Pioneer Accountable Care Organization (ACO) Model. These models have encouraged private payers to adopt similar accountable, value-based care models.
Pay for Performance (P4P)
It is a type of value-based reimbursement that rewards healthcare providers for meeting or exceeding quality, efficiency, or patient health outcomes benchmarks. This system incentivizes providers to deliver high-quality care in a cost-effective manner.
Accountable Care Organizations (ACOs)
ACOs are groups of doctors, hospitals, and other healthcare providers that work together to provide high-quality care to patients while minimizing costs. ACOs are a relatively new concept in healthcare, but they have the potential to revolutionize the way we deliver care.
Here are some of the benefits of ACOs:
- They can improve coordination of care, which can lead to better outcomes for patients.
- They can help to reduce costs by avoiding unnecessary tests and procedures.
- They can give patients more control over their care.
Care Episodes
A care episode is a group of healthcare services that a patient receives for a specific medical condition or during the treatment of a particular illness. It includes everything from the first appointment with the doctor to the follow-up appointment.
This concept is particularly relevant in the context of value-based care. In value-based care, providers are reimbursed based on the quality of care they provide, rather than the number of services they perform. This means that providers have an incentive to provide efficient, high-quality care and avoid unnecessary services.
Care episodes can help providers achieve this goal by providing a holistic view of the patient’s care. This includes all of the patient’s interactions with the healthcare system, from the initial diagnosis to the follow-up care. This information can help providers identify and address any gaps in care, and ensure that the patient receives the best possible care.
Pay-for-Performance Healthcare System
A Pay for Performance (P4P) system incentivizes healthcare providers to meet specified quality and efficiency standards. These benchmarks form the basis of performance assessment, which requires robust data collection and analytics capabilities to accurately capture and analyze performance data. Payments are then adjusted based on this performance. Providers who meet or exceed these benchmarks receive higher payments, while those who fall short may receive lower payments or none, creating a strong financial incentive for providers to improve care quality and efficiency.
Conclusion
There’s no one answer to “how much medical billing services cost.” The prices can change because of different things. But don’t worry, knowing the common pricing ways and what affects the charges can help doctors make good choices. It’s like finding the best balance between value and cost for your healthcare practice. Prices may change as the healthcare system grows. Always try to be efficient and effective in managing your healthcare revenue.