Medicare, known for its strict regulations on claim filing and reimbursement, requires careful adherence to its rules to ensure proper patient care and compliance.
One such regulation is the “Medicare 8-Minute Rule”.
This rule can easily trip you up despite its straightforward name, leading to miscalculations and denied claims.
That’s why we’re here to guide you through the complexities of the Medicare 8-Minute Rule, empowering you to confidently and accurately bill for your therapy services.
What is the 8-Minute Rule?
The 8-Minute Rule was introduced by Medicare in April 2000. This rule determines how long a therapist needs to work to get paid. It is a way for the government healthcare system, Medicare, to make sure therapists are properly paid for the time they spent helping patients. The Medicare 8-Minute Rule applies to time-based CPT codes only.
The following outpatient providers follow the 8-minute Rule when billing Medicare for their services:
- Private practices
- Skilled nursing facilities
- Rehabilitation facilities
- Home health agencies providing therapy covered under Medicare Part B in the home of the beneficiary
- Hospital outpatient departments (including emergency)
Under this Rule:
For time-based codes, a therapist must provide direct treatment for at least 8 minutes in order to receive reimbursement from Medicare.
Basically, when calculating the number of billable units for a particular date of service, Medicare adds up the total minutes of skilled, one-on-one therapy and divides that total by 15.
If 8 or more minutes are left over, the therapist can bill for one more unit; if 7 or fewer minutes remain, the therapist cannot bill an additional unit.
Calculating Units as per the Medicare 8-Minute Rule
Follow these steps to calculate the appropriate number of units for billing:
➜ Step 1 – Add all the time spent on timed services to determine the total number of billable units.
➜ Step 2 – Separate each whole 15-minute unit by CPT code. For instance, 2 units of 97761 would equal 30 minutes.
➜ Step 3 – Handle any remaining minutes that have not been converted into whole units. These are your “remainder minutes,” which can be rounded up to create entire units if at least 8 minutes are remaining.
➜ Step 4 – If a service has 8 remaining minutes left, bill for another unit.
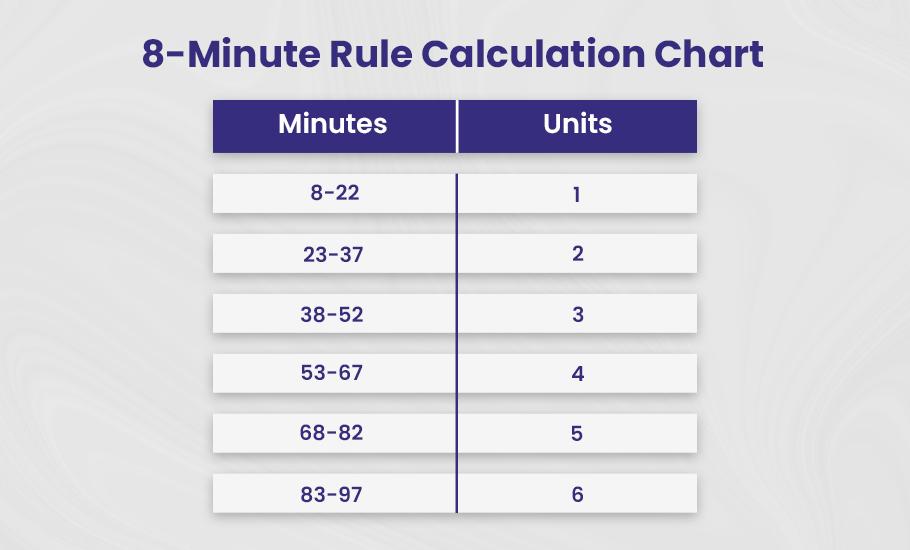
8-Minute Rule Reference Chart
You can bill Medicare for a single “billable unit” of service if it lasts at least eight minutes (up to 22 minutes). After that, you calculate billable units in 15-minute increments.
You must understand that billable units must equal at least 8 minutes of direct patient interaction for timed codes.
You can bill for one unit of a timed code if the total direct time is between 8 and 22 minutes. Two units can be billed if the duration is longer than twenty-two minutes, and so on.
To simplify calculations, CMS provides a chart outlining how many minutes correspond to each billable unit:
| Minutes | Units |
| 8-22 | 1 |
| 23-37 | 2 |
| 38-52 | 3 |
| 53-67 | 4 |
| 68-82 | 5 |
| 83-97 | 6 |
| 98 – 112 | 7 |
| 113 – 127 | 8 |
Examples of Medicare 8-Minute Rule
👉 Example #1
Well now, here we have a situation with a physical therapist and a patient.
The therapist spent 35 minutes doing therapeutic exercises (97110) with the patient. And then another 15 minutes with some manual therapy (97140). So all told, they were working together for 50 minutes.
Now Medicare says you can bill in 15 minute chunks. And any extra minutes left over less than 8 don’t count.
So you take the 50 total minutes and divide by 15. That comes out to 3 whole units of 15 minutes each.
But then we’ve got 5 minutes extra that don’t make a full unit.
Since that 5 minutes is under the 8 minute cutoff, it can’t be billed. The therapist can only bill Medicare for the 3 full 15 minute units here, even though the total time was 50 minutes.
So for this session, all the therapist can bill Medicare for is 3 units of 15 minutes.
That’s the quirky 8-minute rule at work for you. Sure would be nice if we could bill for every minute, but them’s the rules!
Here’s the mathematical calculation for the above example:
- Total Time: 35 + 15 = 50 minutes
- Dividing Total Time by 15: 50 / 15 = 3.3
- Remaining Minutes: 50 – 45 = 5 minutes
- Billing Units: 3 units
👉 Example #2
A speech therapist sat down with the stroke patient and did 35 minutes of cognitive function therapy (97129). Before that, they had tested the patient’s cognitive performance for 55 minutes (96125). All told, the doc spent 90-minutes with the patient that day.
When tallying up the billing, it worked out to:
- 2 units of the 35 minute therapy session (15 minutes each), with 5 minutes remaining
- 3 units of the 55 minute test session (15 minutes each), with 10 minutes to spare
- 1 more unit of the test, since they had that extra 10 minutes (because 10 minutes exceed the 8-minute threshold)
- So in total, 6 billable units for the 90 minutes with the patient.
Timed vs. Service-Based CPT Codes
CPT (Current Procedural Terminology) Codes are standardized codes healthcare professionals use to report various medical services and procedures.
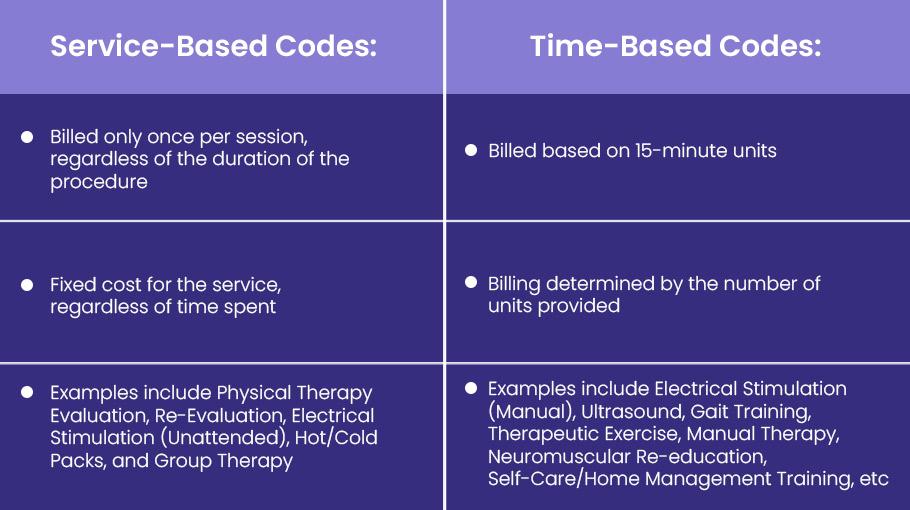
In therapy services, these codes are categorized into two main types:
- Service-Based Codes
- Time-Based Codes
To successfully apply the 8-Minute Rule, you must understand the differences between service- and time-based CPT codes.
➜ Time-Based Codes
Time-Based Codes, often called “Timed Codes,” are billed based on 15-minute units. The actual billing is determined by the number of units provided. For instance: 1 unit = 15 minutes ; 2 units = 30 minutes ; 3 units = 45 minutes.
Examples of Time-Based CPT Codes
- Manual Electrical Stimulation (97032) – Application of electrical stimulation with manual assistance.
- Ultrasound (97035) – Application of therapeutic ultrasound.
- Gait Training (97116) – Training for walking or ambulation, including stair climbing.
- Therapeutic Exercise (97110) – Exercises aimed at improving strength, endurance, and flexibility.
- Manual Therapy (97140) – Hands-on therapy techniques such as joint mobilization and manipulation.
- Neuromuscular Re-education (97112) – Activities that help restore balance, coordination, posture, and kinesthetic sense.
- Self-Care/Home Management Training (97535) – Training for daily living skills and activities.
- Prosthetic Training (97761) – Training for the use of prosthetic devices to improve functionality.
- Physical Performance Test or Measurement (97750) – Evaluation of physical performance through testing.
➜ Service-Based Codes
Service-Based Codes are billed only once per session, irrespective of how long the session or procedure takes. The cost remains fixed regardless of whether the procedure took 10 or 40 minutes.
Examples of Service-Based Codes
- Physical Therapy Re-Evaluation (97164) – Follow-up evaluation to assess progress or modify the treatment plan.
- Unattended Electrical Stimulation (97014) – Electrical stimulation does not require continuous attendance by a provider.
- Hot/Cold Packs (97010) – Application of thermal modalities like hot packs or ice packs.
- Group Therapy (97150) – Therapy is provided in a group setting involving multiple patients.
Appropriate Billing Modifiers
When submitting claims, include any relevant modifiers to impact reimbursement for therapy services:
- CQ/CO: Services performed wholly or partly by a PTA or OTA
- GA: Advanced Beneficiary Notice (ABN) on file for non-coverage
- GO: Services provided by an OT
- GN: Services provided by an SLP
- GP: Services provided by a PT
- KX: Exceeded Medicare therapy threshold but still necessary
- XP: Services billed separately by a different provider
- 22: Increased procedural services
- 52: Reduced services at the provider’s discretion
- 59: Designates services not usually provided together (NCCI edit pairs)
- 95: Telemedicine services
Billing with Mixed Remainders
Mixed remainders refer to leftover minutes from different billing codes.
Example:
- Manual Therapy (97140): 21 minutes
- Gait Training (97116): 17 minutes
Steps:
- 1 unit of 97140 (15 minutes), 1 unit of 97116 (15 minutes)
- Remaining: 6 minutes (97140), 2 minutes (97116)
- Combine remaining minutes to bill another unit of 97140
Management and Assessment Time
If provided one-on-one, therapists can bill for patient management, assessment, and education time.
Billable Activities:
- Assessing response to interventions
- Patient education on self-care
- Answering patient questions
- Documenting in the patient’s presence
💡 Pro Tips for Seamless Compliance to the 8-Minute Rule
➜ Provide regular personnel training and education investments.
➜ Establish thorough documentation practices and conduct routine record audits.
➜ Keep up with any modifications to the physical therapy billing standards or revisions to CMS.
➜ When addressing complicated situations or billing scenarios, get advice from consultants or industry professionals.
AMA’s Rule of Eights vs Medicare 8-Minute Rule
The American Medical Association (AMA) follows the “Rule of Eights,” which requires at least 8 minutes of one-on-one treatment to bill a unit for each CPT code. Unlike CMS, which aggregates time across all codes, the AMA separates the time by individual code.
Example:
8 minutes of therapeutic exercise (97110) and 8 minutes of manual therapy (97140).
Under the AMA Rule of Eights
- 1 unit of 97110
- 1 unit of 97140
Under the CMS 8-Minute Rule
- Only 1 unit of either 97110 or 97140 can be billed due to the aggregated total of 16 minutes.
The Difficulty of Medicare’s 8 Minute Rule for Therapists: An Urgent Warning and Solution
For therapists, Medicare’s 8 Minute Rule is as troublesome as it is necessary. Bill the wrong units and your pay suffers. Bill too many and you’re penalized for upcoding. It’s a tricky business, and many find themselves caught between a rock and a hard place, unsure of the right path forward.
The threat is real, but the solution is simple. The medical billing experts at BellMedEx have mastered Medicare’s 8 Minute Rule. Our team of highly-trained billers ensure 100% accuracy in unit submissions, protecting your pay and avoiding penalties.
Want to see our medical billing service in action? Schedule a free demo. We’ll walk you through how we navigate Medicare’s 8 Minute Rule and get you the most from each claim.