Denials in healthcare claims are a growing challenge, costing providers time, money, and patient trust. Average denial rates are reaching up to 15% and nearly 90% of those denials are preventable. That’s why effective healthcare denial management is not optional, it’s a must!
Effective claim denial management starts with proven strategies to reduce denial rates, recover lost revenue, and streamline operations. This guide covers the best practices for effective denials management in healthcare and medical billing.
But first, what is denial management, and why is it important anyway?
What is a Healthcare Denial Management Process?
Denial Management Process in healthcare is the process where healthcare providers, medical billing teams, and medical revenue cycle management experts identify, analyze, and resolve denied insurance claims from payers. These payers may be Medicare, Medicaid or commercial insurers like BCBS, Elevance Health, and more.
A medical claim can be denied for many reasons, including out-of-network providers, incorrect or missing information, non-covered claims, duplicate claims, and lack of medical necessity.
An effective healthcare denial management process involves finding the reason for each denial, correcting errors such as coding mistakes or missing documentation, and appealing claims when needed.
The goal is to recover lost revenue, prevent future denials, and ensure proper reimbursement. This process uses tools like electronic remittance advice (ERA), explanation of benefits (EOB), and automation software to track and manage denials efficiently.
Why Denial Management Process is Important?
A denial management process protects healthcare organizations from major financial losses caused by denied claims. It also helps maintain steady cash flow and supports the ability to deliver quality patient care.
Denial rates of 10-15% occur in almost every healthcare practice in the US. Effective healthcare denial management maximizes revenue. It also improves your practice’s finances by cutting revenue cycle costs and reducing administrative burdens.
With fewer denials to worry about, you can focus on enhancing overall hospital or practice efficiency. Smooth denial management reduces errors and streamlines workflows. It helps you spend more time on patient care and building genuine relationships.
15+ Best Practices for an Effective Denial Management Process in Healthcare
An effective claim denial management process starts with checking insurance eligibility upfront. It also involves improving paperwork accuracy and using automation tools to streamline processes. Creating effective appeal processes helps resolve denials quickly.
Providers must ensure documentation is accurate and complete, obtain necessary prior authorizations, and apply up-to-date coding standards. Regular audits and staff training catch medical billing errors early.
Best practices for effective claims denial management process includes the following:
- Review Denials Promptly to Determine Root Causes
- Standardize the Appeals Process Across All Departments
- Create and Maintain a Comprehensive Appeals Checklist
- Track, Categorize, and Analyze Denial Trends Regularly
- Implement Proactive Denial Prevention Measures
- Examine Historical Denials to Identify Systemic Issues
- Develop and Document Clear Denials Management Strategies
- Verify Patient Information, Insurance Eligibility, and Benefits Pre-Service
- Double Check Referrals and Prior Authorizations Before Treatment
- Ensure Accurate, Complete, and Timely Documentation and Coding
- Conduct Regular Internal Audits of Claims and Documentation
- Educate and Train Staff on Payer Guidelines, Coding Rules, and Updates
- Establish a Dedicated Healthcare Denial Management and Appeals Team
- Monitor Denials and Appeals Using Key Performance Indicators (KPIs)
- Enhance Documentation Practices to Justify Medical Necessity
- Implement Advanced Claims Scrubbing Before Submission
- Use Ongoing Revenue Cycle Management (RCM) Analysis to Identify Gaps
- Strengthen Communication Between Billing, Clinical, and Admin Teams
- Leverage Technology, Automation, and RCM Tools to Streamline Workflows
- Outsource to Revenue Cycle Experts for Complex or High-Volume Denials
- Streamline Medical Billing Processes to Minimize Human Error
- Strengthen Payer Relationships Through Consistent Communication
- Apply Data-Driven Insights to Optimize Denial Responses and Appeals
1). Review Denials Promptly to Determine Root Causes
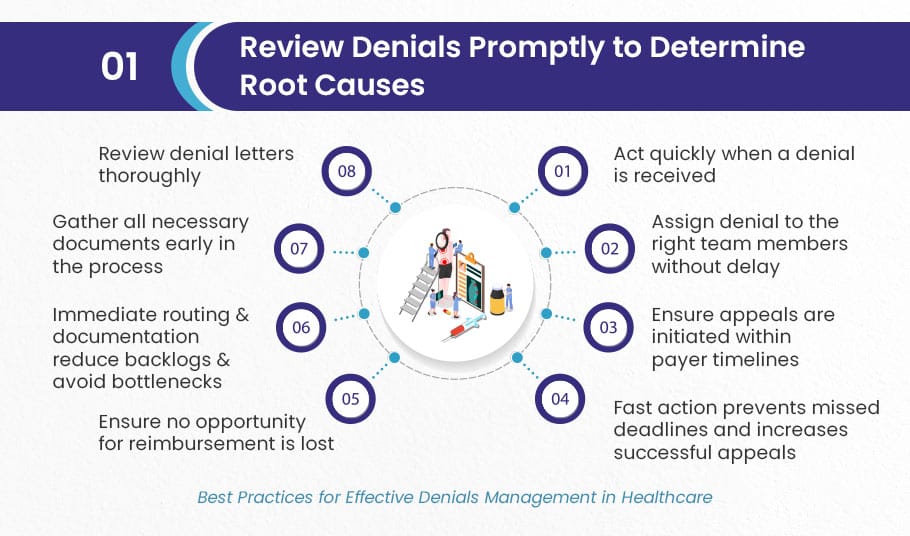
Act quickly when a denial is received. Assign it to the right team members without delay to ensure appeals are initiated within payer timelines. Fast action helps prevent missed deadlines and increases the chances of successful appeals. Review denial letters thoroughly and gather all necessary documents early in the process. Immediate routing and documentation reduce backlogs, avoid bottlenecks, and ensure no opportunity for reimbursement is lost.
2). Standardize the Appeals Process Across All Departments
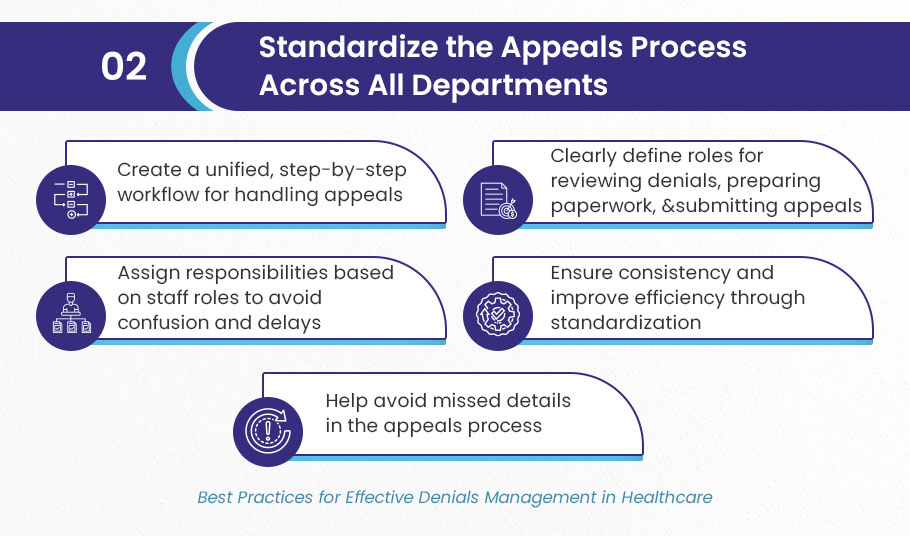
Create a unified, step-by-step workflow for handling appeals across your team. Clearly define who reviews denials, who prepares paperwork, and who submits the appeal. Assign responsibilities based on staff roles to avoid confusion or delays. Standardization ensures consistency, improves efficiency, and helps avoid missed details. Include training for staff to stay current on payer-specific appeal requirements and documentation standards.
3). Create and Maintain a Comprehensive Appeals Checklist
Develop a detailed checklist to guide your team through each appeal submission. Include all necessary components, forms, denial explanation, appeal letters, supporting documents, and insurer communication logs. This checklist minimizes errors and missed items that could lead to a second denial. Keeping it updated with payer-specific nuances helps staff stay aligned and confident when building appeal packets, which improves turnaround time and approval rates.
4). Track, Categorize, and Analyze Denial Trends Regularly
Collect and study denial data by payer, service type, denial code, and department. Identify recurring causes and patterns behind your denials. Track metrics like first-pass denial rates, appeal success rates, and time to resolution. Analyzing this data uncovers inefficiencies and highlights opportunities for training, workflow improvement, or system upgrades. It turns your healthcare denial management from reactive to proactive, driving long-term financial gains.
5). Implement Proactive Denial Prevention Measures
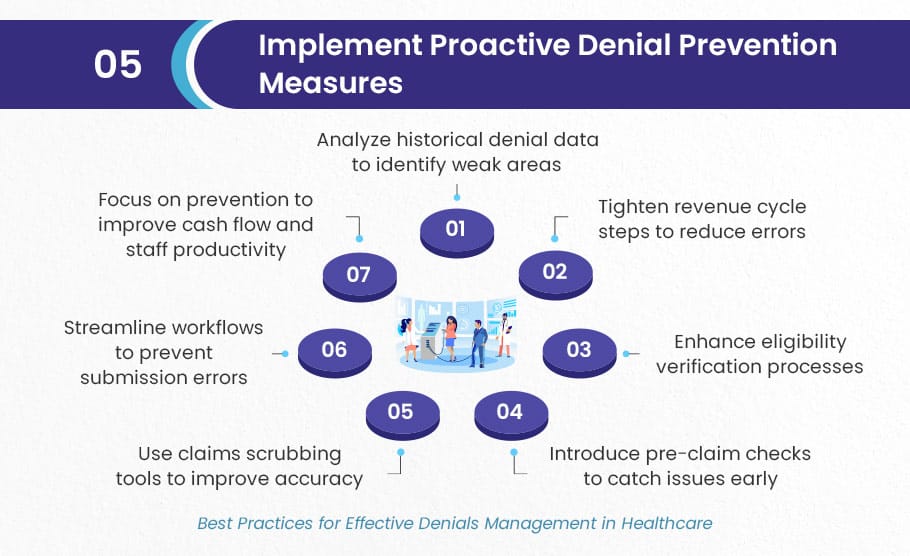
Prevent denials before they happen by tightening every step in your revenue cycle. Use historical denial data to target weak areas, like inaccurate coding or incomplete documentation. Introduce pre-claim checks, claims scrubbing tools, and better eligibility verification. Streamline processes so errors are caught before submission. Prevention is less costly and more effective than handling denials after the fact, and it directly improves cash flow and staff productivity.
6). Examine Historical Denials for Recurring Issues
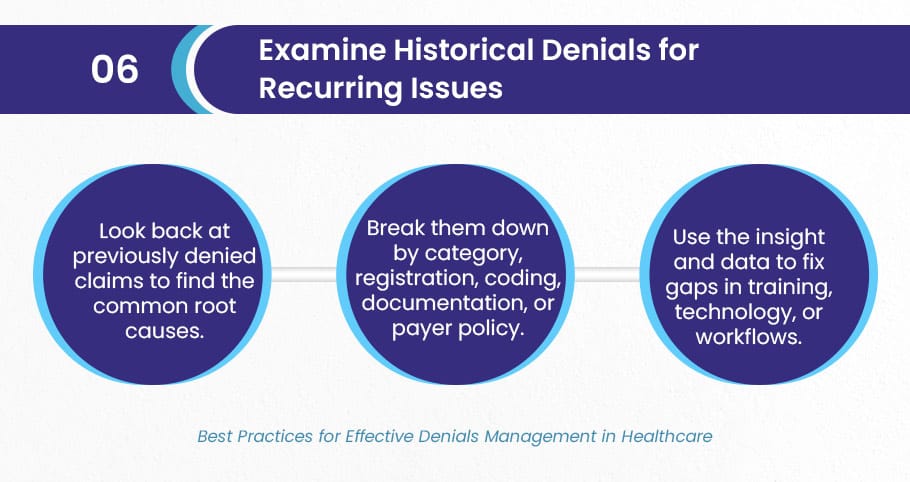
Look back at previously denied claims to find the common root causes. Break them down by category, registration, coding, documentation, or payer policy. Use this insight to fix gaps in training, technology, or workflows. Conducting this analysis regularly helps catch trends early and refine processes before errors multiply. It’s a critical step in building a data-driven, continuously improving denial prevention strategy.
7). Develop and Document Clear Denials Management Strategies
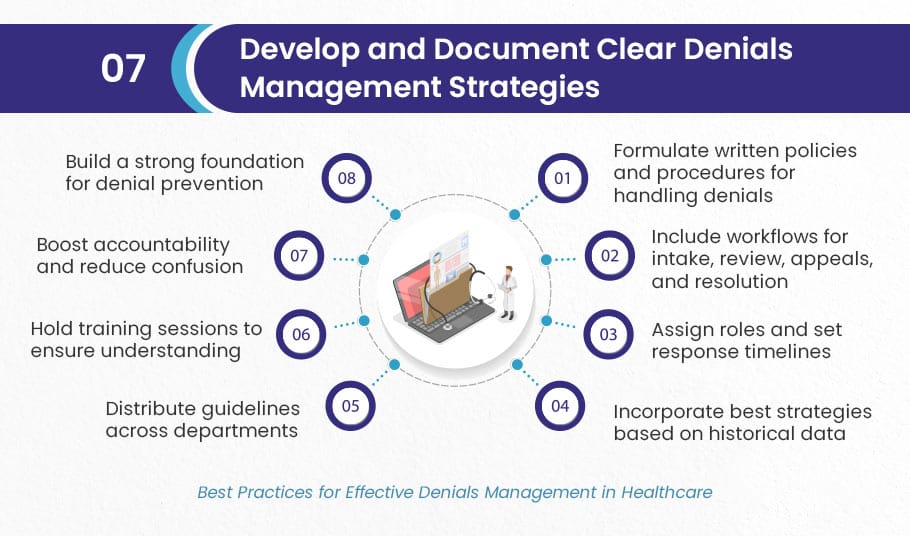
Formulate written policies and procedures that guide how your team handles denials. Include workflows for intake, review, appeals, and resolution. Assign roles, set response timelines, and include best strategies based on historical data. Distribute these guidelines across departments and hold training sessions to ensure everyone understands them. A documented strategy boosts accountability, reduces confusion, and builds a strong foundation for denial prevention.
8). Verify Patient Information, Insurance Eligibility, and Benefits Pre-Service
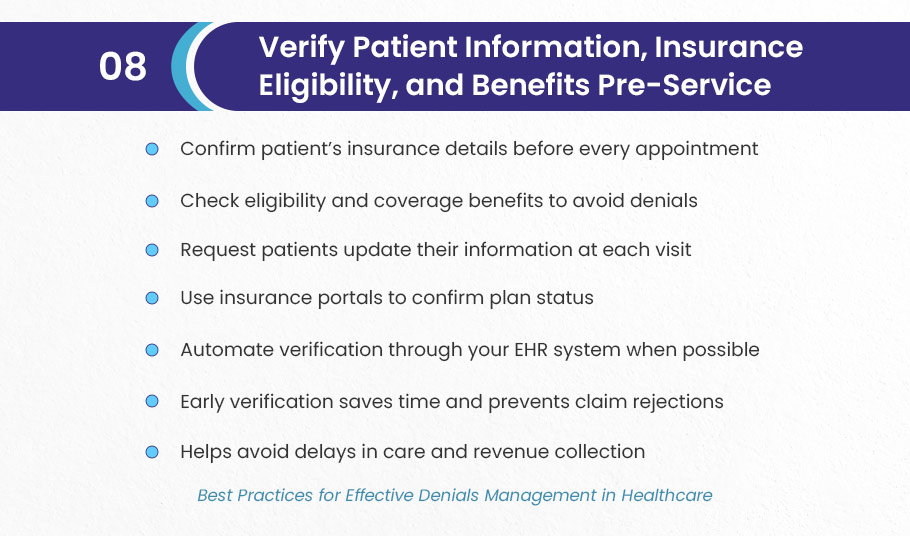
Before every appointment, confirm the patient’s insurance details, eligibility, and coverage benefits. Inaccurate or outdated information is one of the leading causes of denials. Ask patients to update their information during each visit and check insurance portals to confirm plan status. Automate this where possible through your EHR. Verifying early saves time and prevents rejections that can delay care and revenue.
9). Double Check Referrals and Prior Authorizations Before Treatment

Ensure that referrals and prior authorizations are complete, current, and match the services to be provided. Errors here cause up to 18% of all denials. Build workflows where front-desk or pre-authorization staff verify the correct procedure, authorization number, and expiration date. Educate staff on how to resolve common issues. Accurate authorization management improves claim approval rates and strengthens payer trust.
10). Perform Ongoing Revenue Cycle Management (RCM) Analysis
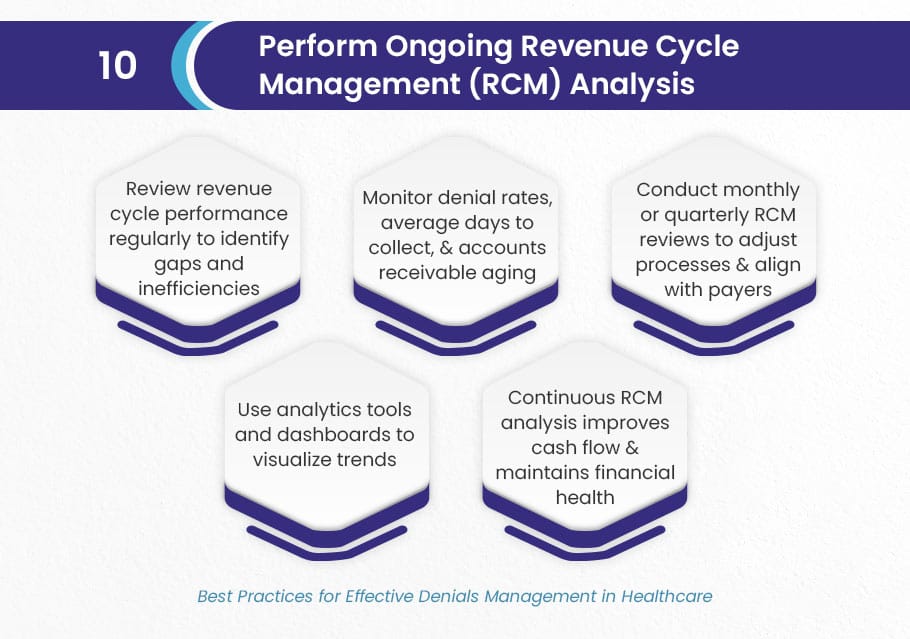
Review your revenue cycle performance regularly to find gaps and inefficiencies. Monitor metrics like denial rates, average days to collect, and accounts receivable aging. Monthly or quarterly RCM reviews help you adjust processes, align with payer changes, and improve cash flow. Use analytics tools and dashboards to visualize trends. Continuous RCM analysis keeps your practice financially healthy and responsive to evolving challenges.
11). Ensure Accurate, Complete, and Timely Documentation and Coding
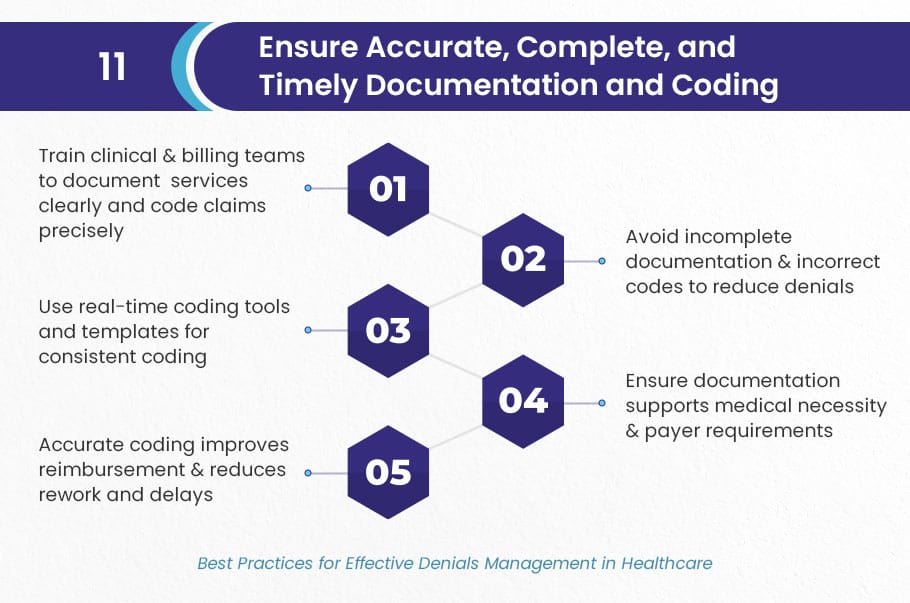
Train your clinical and billing teams to document services clearly and code claims precisely. Incomplete documentation or incorrect codes are major reasons for both technical and clinical denials. Use real-time coding tools and templates to help staff code more consistently. Make sure documentation supports medical necessity and includes every detail required by payers. Accurate coding not only improves reimbursement but also reduces costly rework and delays.
12). Conduct Regular Internal Audits of Billing and Documentation
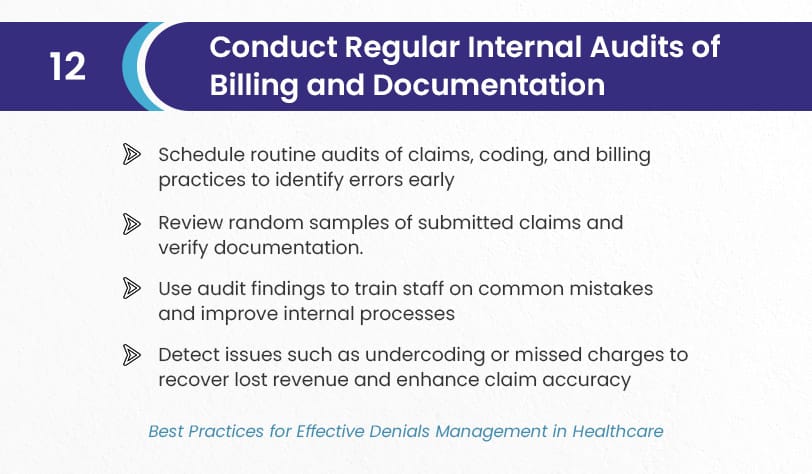
Schedule routine audits of your claims, coding, and billing practices to spot errors before they lead to denials. Review random samples of submitted claims and cross-check documentation for compliance and accuracy. Use audit results to train staff on common mistakes and update internal processes. Audits also help uncover issues like undercoding or missed charges, giving your practice a chance to recover lost revenue and boost claim accuracy.
13). Educate and Train Staff on Payer Guidelines and Denials Prevention
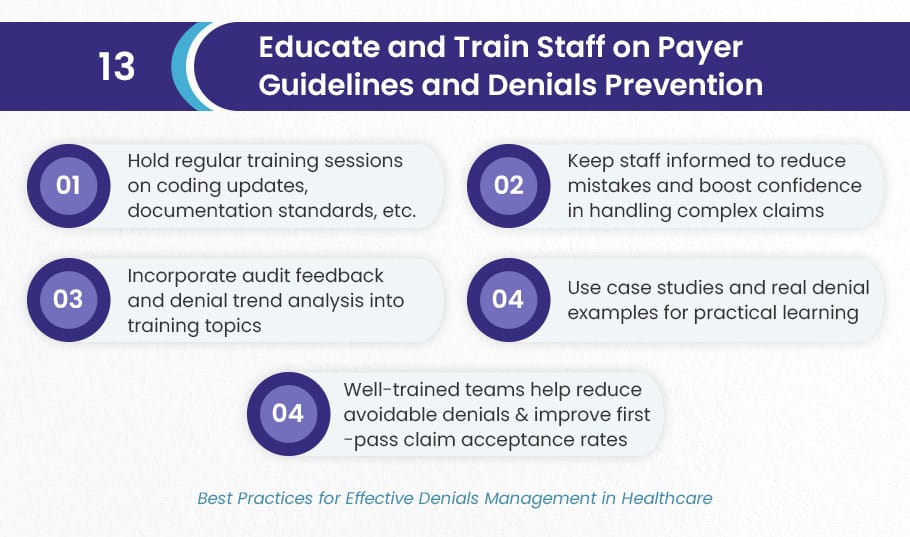
Hold regular training sessions to keep staff informed about coding updates, documentation standards, and payer-specific rules. Educated staff make fewer mistakes and feel more confident handling complex claims. Incorporate feedback from audits and denial trend analysis into training topics. Use case studies and real denial examples for hands-on learning. Well-trained teams reduce avoidable denials and increase first-pass claim acceptance rates.
14). Establish a Dedicated Healthcare Denial Management and Appeals Team
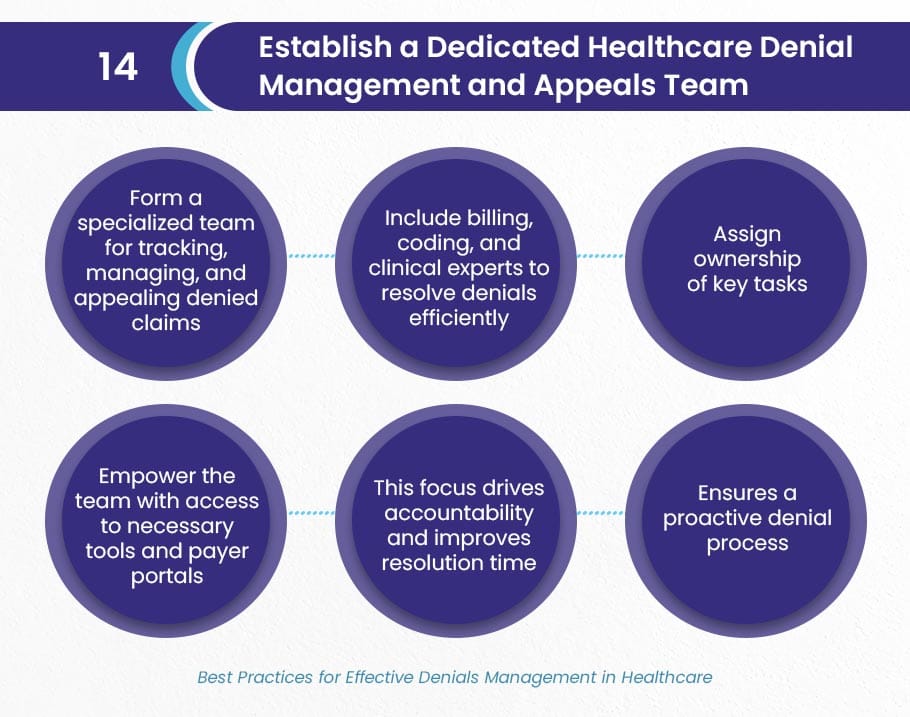
Form a specialized team focused solely on tracking, managing, and appealing denied claims. Include billing, coding, and clinical experts who can collaborate to resolve denials efficiently. Assign ownership of key tasks and empower the team with access to necessary tools and payer portals. This focus drives accountability, improves resolution time, and ensures the denial process is handled proactively, not reactively.
15). Monitor Denials Using Key Performance Indicators (KPIs)
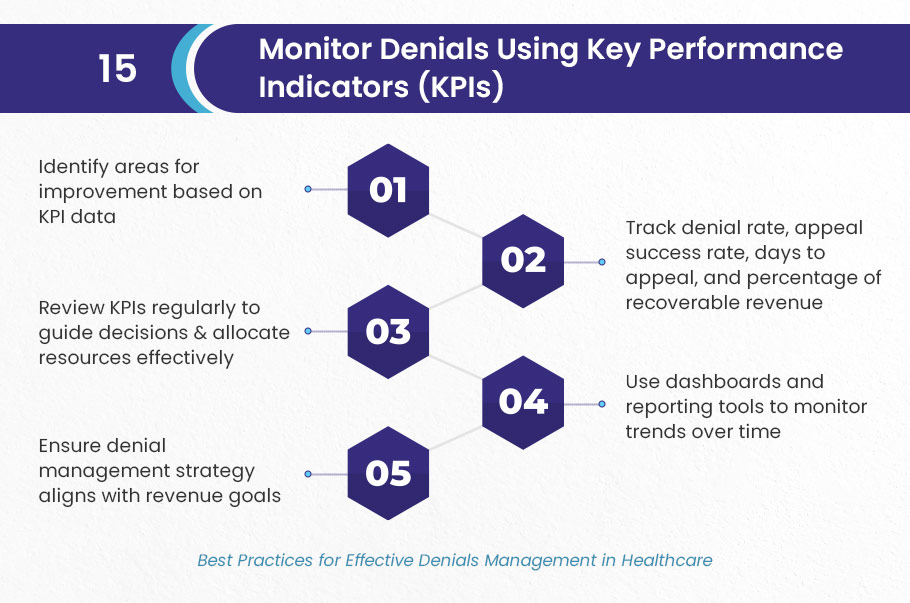
Track KPIs like denial rate, appeal success rate, days to appeal, and percentage of recoverable revenue. These metrics provide a clear picture of how well your healthcare denial management process is performing. Use dashboards and reporting tools to monitor trends over time and identify improvement areas. Reviewing KPIs regularly helps guide decisions, allocate resources wisely, and ensure your denial strategy stays aligned with revenue goals.
16). Enhance Clinical and Administrative Documentation Practices
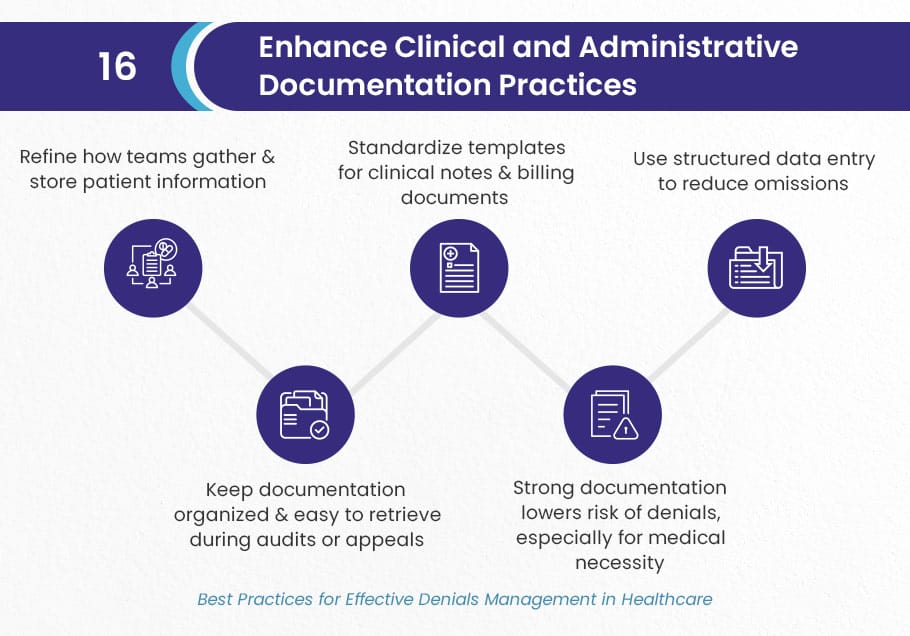
Refine how your teams gather and store patient information. Standardize templates for clinical notes and billing documents. Use structured data entry whenever possible to reduce omissions. Keep your documentation organized and easy to retrieve during audits or appeals. Strong documentation reduces the likelihood of denials, especially those related to medical necessity.
17). Implement Robust Claims Scrubbing Before Submission
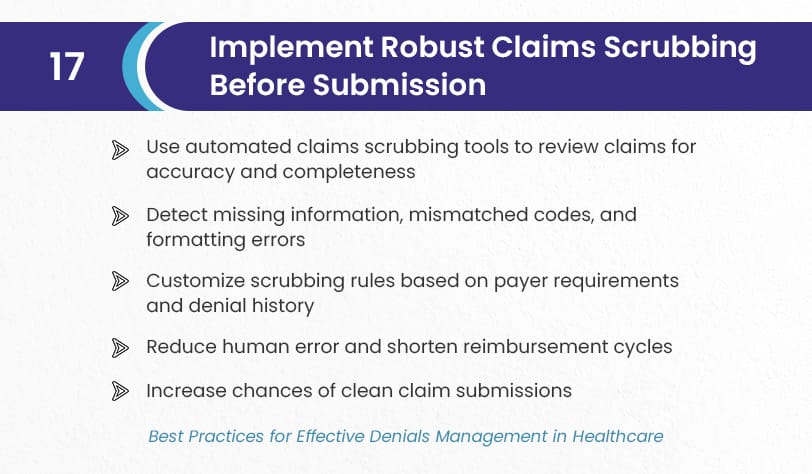
Use automated claims scrubbing tools to review claims for accuracy and completeness before submission. These tools catch missing information, mismatched codes, and formatting errors that commonly cause denials. Customize rules based on payer requirements and denial history. A strong scrubbing process reduces human error, shortens reimbursement cycles, and increases the chances of clean claim submissions.
18). Maintain Clear and Consistent Communication Between Departments
Encourage regular communication between billing, coding, clinical, and front-desk teams. Use shared notes, internal messaging tools, and routine check-ins to discuss complex cases or frequent denial triggers. When teams share knowledge, they can work together to prevent repeat issues. Clear internal communication leads to faster resolution of claim issues and creates a more coordinated denial prevention effort.
19). Leverage Revenue Cycle Management (RCM) Technology and Automation
Adopt advanced RCM tools that automate claims tracking, eligibility checks, denial flagging, and appeals. Automation reduces manual workloads, speeds up follow-ups, and keeps your billing team focused on higher-value tasks. Look for systems with analytics features that help pinpoint where denials occur. Investing in RCM tech increases accuracy, saves time, and gives you real-time insight into your revenue flow.
20). Apply Data-Driven Insights to Optimize Denial Responses
Use analytics to drive smarter decisions. Examine success rates of past appeals, identify high-denial services, and assess which payers deny most frequently. This data can inform training, refine documentation standards, and focus resources where they’ll have the biggest impact. Data doesn’t just tell you what went wrong, it tells you how to fix it for good.
21). Streamline Medical Billing Workflows to Reduce Human Error
Simplify your billing processes to reduce complexity and minimize mistakes. Map out your current workflow and identify steps that cause delays or confusion. Use automation where possible and remove duplicate tasks. Clear workflows help ensure claims are submitted correctly the first time, reduce denials, and allow staff to handle more cases in less time.
22). Strengthen Payer Relationships Through Open Dialogue
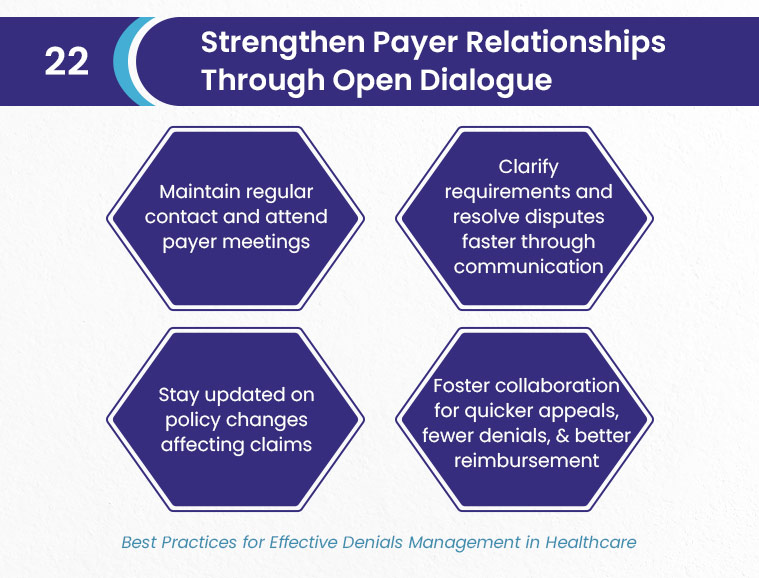
Build strong working relationships with insurance payers by maintaining regular contact and attending payer meetings. Open communication allows your team to clarify requirements, resolve disputes faster, and stay informed about policy changes. Collaborative relationships with payers can also lead to quicker appeals, fewer denials, and even better reimbursement.
23). Hire a Medical Billing Company for Your Denial Management
Partner with healthcare denial management specialists who partner with hospitals, practices, and other healthcare entities. Experienced medical billing companies like BellMedEx bring deep industry expertise and efficient systems to reduce your denial rate.
Outsourcing can free up internal resources, boost recovery rates, and ensure complex claims are handled professionally. It’s a smart move for medical practitioners that want better results without stretching their teams too thin.




