1 in 3 Americans is covered by Blue Cross Blue Shield (BCBS), making it an important player for most therapy practices. BCBS operates through 33 independent companies across the US, each with varying policies. That’s why it’s extremely important to know how much Blue Cross Blue Shield pays for therapy and mental health services.
This guide helps therapy and mental health providers understand BCBS reimbursement for therapy services across different states. This will help optimize payments, avoid medical billing errors, and manage insurance complexities. Let’s dive in!
Understanding the Ins and Out of Therapy Reimbursement
Reimbursement means getting paid by insurance after providing therapy. As a provider, you send a claim to Blue Cross Blue Shield for each session. They then pay you based on your contract or the patient’s plan. If you’re in-network, BCBS usually pays more and faster. If you’re out-of-network, payments are lower, and the process is slower.
Key Terms Every Provider Should Know
- The billed amount is what you charge.
- The allowed amount is what BCBS agrees to pay.
You get paid based on that allowed amount, minus any copay, coinsurance, or deductible the patient owes.
- In-network means you have a contract with BCBS and follow their rates.
- Out-of-network means no contract, which may lead to higher patient costs and more paperwork for you.
Always check your network status in each state where you practice.
Common Challenges Mental Health Therapists Face
- BCBS reimbursement isn’t always smooth.
- Providers often deal with delayed payments, claim denials, or partial reimbursements.
- Each state’s BCBS company may follow different rules.
- Keeping up with their requirements takes time.
- Missed coding or documentation issues can also delay or reduce payment.
- To stay on top, know your local BCBS policies and track each claim carefully.
How Much Does Blue Cross Blue Shield Reimburse for Therapy (Mental Health)?
Blue Cross Blue Shield reimburses therapy costs based on the patient’s coverage details like deductibles, copays, or coinsurance. In-network therapists generally have lower copays, ranging from $15 to $80 per session. Some plans allow coverage before the deductible is met, while others require patients to pay the full session fee until the deductible is reached.
| Procedure | CPT Code | Estimated BCBS Reimbursement (per session) | Additional Notes |
| Psychiatric Diagnostic Evaluation | 90791 | $150 – $300 | Initial evaluation, often for new patients. |
| Psychotherapy, 30 minutes | 90832 | $60 – $120 | Common for shorter sessions, may vary by region. |
| Psychotherapy, 45 minutes | 90834 | $80 – $140 | Typical session length for ongoing therapy. |
| Psychotherapy, 60 minutes | 90837 | $100 – $160 | Longer sessions for more complex therapy. |
| Family Therapy (without patient) | 90846 | $90 – $150 | Therapy focused on family dynamics, no patient present. |
| Family Therapy (with patient) | 90847 | $100 – $170 | Family therapy with patient involved in the session. |
| Group Psychotherapy | 90853 | $30 – $70 | Shared therapy with multiple clients in a group setting. |
| Crisis Psychotherapy, 60 minutes | 90839 | $120 – $200 | Immediate therapy for mental health crises. |
| Add-on for Crisis Psychotherapy | 90840 | $50 – $100 | Used in addition to 90839 for extended crisis therapy. |
| Telehealth Counseling | Varies | $50 – $110 | Online therapy sessions, reimbursement varies by plan. |
| Psychiatric Diagnostic Evaluation (Interactive) | 90792 | $180 – $350 | Used when the evaluation is interactive with patient. |
| Psychological Testing (Per Hour) | 96130 | $150 – $250 | Comprehensive testing for mental health conditions. |
| Neuropsychological Testing | 96136 | $250 – $400 | In-depth assessments of cognitive functions. |
| Add-on for Neuropsychological Testing | 96137 | $100 – $150 | Add-on for additional testing services. |
| Individual Counseling / Online Therapy (Telehealth) | 90832-90837 (telehealth) | $60 – $130 | Variable based on plan, includes all teletherapy services |

Remember, these are just the estimates!
Reimbursement rates for therapy vary widely depending on where you practice. Since BCBS is made up of 33+ independent companies across the US, each with its own fee schedules and policies, rates can shift from one state to another, even for the same CPT code.
If you’re a therapy provider, knowing these state-specific benchmarks can help you:
- Set realistic rates.
- Negotiate better contracts with BCBS.
- Decide whether going in-network is financially worthwhile.
- Understand potential revenue when expanding to new states or offering telehealth.
BCBS Therapy Reimbursement Rates (State-wise)
The below-given table provides real-world estimates for 60-minute psychotherapy sessions (CPT Code 90837) across all 50 states, based on provider reports, claims data, and BCBS regional trends. These figures are approximate and can vary based on specific BCBS affiliates, provider contracts, and geographic regions within each state.
| State | In-Network Rate (USD) | Out-of-Network Rate (USD) | BellMedEx Billers’ Notes |
| Alabama | $85–$95 | $70–$85 | Rates vary by region; urban areas may see higher reimbursements. |
| Alaska | $110–$125 | $90–$110 | Higher rates due to limited provider availability. |
| Arizona | $100–$115 | $80–$100 | Competitive rates; urban centers like Phoenix may offer higher reimbursements. |
| Arkansas | $80–$90 | $65–$80 | Rural areas may experience lower rates; urban centers provide higher reimbursements. |
| California | $100–$120 | $80–$100 | Significant variation; urban areas like San Francisco and Los Angeles offer higher rates. |
| Colorado | $95–$105 | $75–$95 | Rates are competitive; the Denver area may have slightly higher reimbursements. |
| Connecticut | $105–$115 | $85–$105 | Higher rates in urban areas; rural regions may see slightly lower reimbursements. |
| Delaware | $90–$100 | $70–$90 | Rates are consistent across the state. |
| Florida | $95–$105 | $75–$95 | Urban areas like Miami and Orlando offer higher reimbursements. |
| Georgia | $85–$95 | $70–$85 | Rates vary by region; metropolitan areas may have higher reimbursements. |
| Hawaii | $115–$125 | $95–$115 | Higher rates due to limited provider availability. |
| Idaho | $75–$85 | $60–$75 | Rural areas may experience lower rates; urban centers provide higher reimbursements. |
| Illinois | $100–$110 | $80–$100 | The Chicago area offers higher reimbursements; rates vary in other regions. |
| Indiana | $85–$95 | $70–$85 | Rates are consistent across the state. |
| Iowa | $80–$90 | $65–$80 | Rural areas may experience lower rates; urban centers provide higher reimbursements. |
| Kansas | $75–$85 | $60–$75 | Rates vary by region; urban areas may have higher reimbursements. |
| Kentucky | $80–$90 | $65–$80 | Rates are consistent across the state. |
| Louisiana | $85–$95 | $70–$85 | Urban areas like New Orleans offer higher reimbursements. |
| Maine | $90–$100 | $70–$90 | Rates are consistent across the state. |
| Maryland | $100–$110 | $80–$100 | Higher rates in urban areas; rural regions may see slightly lower reimbursements. |
| Massachusetts | $110–$120 | $90–$110 | Higher rates in urban areas like Boston; rural regions may see slightly lower reimbursements. |
| Michigan | $95–$105 | $75–$95 | Rates vary by region; metropolitan areas offer higher reimbursements. |
| Minnesota | $90–$100 | $70–$90 | Rates are consistent across the state. |
| Mississippi | $80–$90 | $65–$80 | Rural areas may experience lower rates; urban centers provide higher reimbursements. |
| Missouri | $85–$95 | $70–$85 | Rates vary by region; urban areas may have higher reimbursements. |
| Montana | $75–$85 | $60–$75 | Rural areas may experience lower rates; urban centers provide higher reimbursements. |
| Nebraska | $80–$90 | $65–$80 | Rates vary by region; urban areas may have higher reimbursements. |
| Nevada | $90–$100 | $70–$90 | Rates are consistent across the state. |
| New Hampshire | $95–$105 | $75–$95 | Higher rates in urban areas; rural regions may see slightly lower reimbursements. |
| New Jersey | $105–$115 | $85–$105 | Higher rates in urban areas like Newark and Jersey City; rural regions may see slightly lower reimbursements. |
| New Mexico | $85–$95 | $70–$85 | Rates vary by region; urban areas may have higher reimbursements. |
| New York | $110–$120 | $90–$110 | Significant variation; urban areas like New York City offer higher rates. |
| North Carolina | $90–$100 | $70–$90 | Rates are consistent across the state. |
| North Dakota | $75–$85 | $60–$75 | Rural areas may experience lower rates; urban centers provide higher reimbursements. |
| Ohio | $85–$95 | $70–$85 | Rates vary by region; metropolitan areas offer higher reimbursements. |
| Oklahoma | $80–$90 | $65–$80 | Rates are consistent across the state. |
| Oregon | $100–$110 | $80–$100 | Higher rates in urban areas like Portland; rural regions may see slightly lower reimbursements. |
| Pennsylvania | $95–$105 | $75–$95 | Rates vary by region; urban areas may have higher reimbursements. |
| Rhode Island | $90–$100 | $70–$90 | Rates are consistent across the state. |
| South Carolina | $85–$95 | $70–$85 | Rates vary slightly between Charleston and other metro regions. |
| South Dakota | $75–$85 | $60–$75 | Rural providers may face lower rates; limited data for urban regions. |
| Tennessee | $85–$95 | $70–$85 | Nashville providers typically receive higher rates than rural counterparts. |
| Texas | $90–$105 | $70–$90 | Rates vary significantly by city; Dallas and Austin are generally higher. |
| Utah | $85–$95 | $70–$85 | Salt Lake City rates are slightly higher; rural areas below average. |
| Vermont | $95–$105 | $75–$95 | Consistent rates across the state due to a small provider base. |
| Virginia | $95–$105 | $75–$95 | Urban areas like Northern Virginia often receive higher reimbursement. |
| Washington | $100–$110 | $80–$100 | Seattle area rates are higher; telehealth rates on par with in-person. |
| West Virginia | $80–$90 | $65–$80 | Lower end of national average; limited provider network. |
| Wisconsin | $90–$100 | $70–$90 | Metro areas such as Madison and Milwaukee pay more than rural regions. |
| Wyoming | $80–$90 | $65–$80 | Small market, but rates are stable; may be influenced by parity laws. |
Factors Influencing BCBS Therapy Reimbursement Rates for Providers
In-network rates are based on negotiated contracts with local BCBS affiliates. Out-of-network payouts are often a percentage of the plan’s “allowed amount” (typically 60–80%) and subject to balance billing. Urban providers generally receive slightly better reimbursements due to market demand and parity compliance. Let us quickly discuss the many factors that affect how much BCBS reimburses for therapy services.
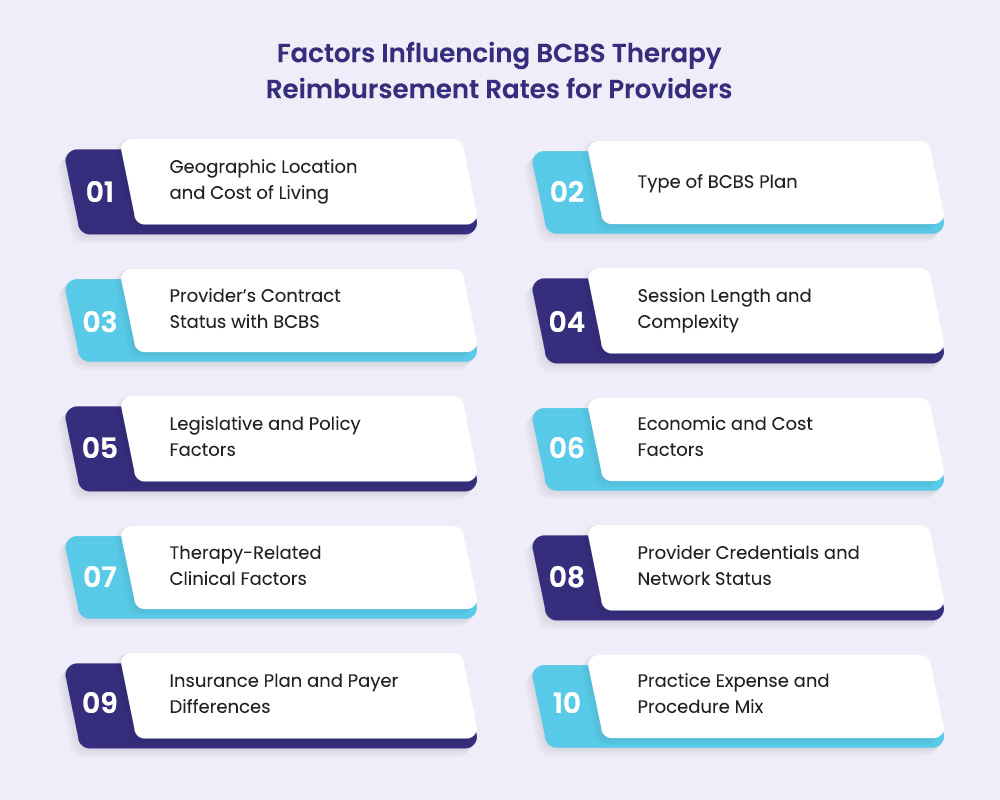
1. Geographic Location and Cost of Living
Reimbursement rates often reflect the local cost of living and provider density. Urban areas with higher living costs and more providers may offer higher rates to attract professionals. And rural areas might offer increased rates to incentivize providers to serve underserved populations.
2. Type of BCBS Plan
The specific BCBS plan type, such as PPO, HMO, or HDHP, can influence reimbursement rates. PPO plans often provide higher reimbursement rates due to their broader network flexibility, whereas HMO plans may offer lower rates but with more controlled access to services.
3. Provider’s Contract Status with BCBS
Providers contracted with BCBS typically receive higher reimbursement rates compared to out-of-network providers. In-network status ensures adherence to negotiated rates and reduces administrative burdens, leading to more predictable payments.
4. Session Length and Complexity
The duration and complexity of therapy sessions directly impact reimbursement rates. Longer sessions or those involving complex therapeutic techniques may warrant higher reimbursement due to the increased time and expertise required.
5. Legislative and Policy Factors
Legislative actions, such as changes in Medicare payment policies, can significantly affect reimbursement rates. For example, the Centers for Medicare & Medicaid Services (CMS) has implemented reductions in the Medicare conversion factor, leading to decreased payments for services unless offset by legislative intervention.
6. Economic and Cost Factors
Economic indices, like the Medicare Economic Index (MEI), reflect the rising costs of providing services. However, reimbursement rates may not always align with these increases due to budget constraints, potentially leading to financial strain for providers.
7. Therapy-Related Clinical Factors
The type of therapy provided influences reimbursement rates. Specialized services, such as psychiatric evaluations or neuropsychological testing, often command higher reimbursement due to their complexity and resource requirements.
8. Provider Credentials and Network Status
Providers with advanced qualifications such as, LCSW, PsyD, or MD may receive higher reimbursement rates due to their expertise. Additionally, being in-network with BCBS can lead to better reimbursement rates compared to out-of-network providers.
9. Insurance Plan and Payer Differences
Reimbursement rates vary among different insurance panels and plans. For instance, Medicare Advantage plans have seen reimbursement increases, while traditional Medicare rates have declined, highlighting the differences in payer policies.
10. Practice Expense and Procedure Mix
The reimbursement impact of changes in practice expenses depends on the share of Relative Value Units (RVUs) attributed to practice expenses for a given service. Services with a higher practice expense share may experience more significant reimbursement changes when adjustments are made.
How Telehealth Affects How Much Does Blue Cross Blue Shield Reimburse for Therapy?
Telehealth has become a key component of therapy services, especially post-COVID-19. BCBS now reimburses telehealth sessions, typically at rates similar to in-person therapy. However, reimbursement can vary based on location, therapy type, and the specific BCBS plan. Some regions may offer lower rates for telehealth, so providers must be aware of these differences.
BCBS Telehealth Reimbursement Policies
State-specific telehealth parity laws impact BCBS reimbursement policies. These laws require BCBS to reimburse telehealth sessions at the same rate as in-person visits, but the rules differ by state. Mental health and therapy providers should check local telehealth regulations and ensure they follow BCBS’s policies when submitting claims.
How to Ensure Telehealth Claims Are Paid Correctly
To ensure correct reimbursement for telehealth, therapists must use the correct billing codes, such as the “GT” modifier for telehealth services. It’s crucial to verify patient eligibility, document sessions thoroughly, and apply the right modifiers and CPT codes. Following these practices helps avoid claim denials and delays, ensuring timely reimbursement for virtual therapy sessions.
How BCBS Plans and Their Therapy Coverage Compare
Blue Cross Blue Shield offers a variety of health insurance plans, each with unique structures and therapy coverage options. Understanding how these plans compare is essential for providers seeking to navigate reimbursement processes.
1. HMO (Health Maintenance Organization) Plans
HMO plans require members to use in-network providers and often need a referral from a primary care physician (PCP) for therapy. Therapy coverage is generally limited to in-network services, except for emergencies. These plans tend to have lower premiums and out-of-pocket costs, but the flexibility is restricted.
2. PPO (Preferred Provider Organization) Plans
PPO plans offer more flexibility, allowing members to see out-of-network providers, though at a higher cost. Therapy services are typically covered, with better rates for in-network visits. Members can still access therapy outside the network, but at higher out-of-pocket costs and lower reimbursement rates for providers.
3. EPO (Exclusive Provider Organization) Plans
EPO plans are similar to PPOs but only cover in-network therapy services. They do not require a referral from a PCP to see a therapist, which offers more convenience for patients. However, out-of-network therapy is not covered under EPO plans, making it important for providers to ensure they are in-network to receive reimbursement.
4. POS (Point of Service) Plans
POS plans require a PCP referral for therapy services but offer some flexibility to access out-of-network care. Therapy is covered, but costs are lower when providers are in-network. Out-of-network services may be reimbursed, but at a higher cost to the patient and potentially lower reimbursement to the provider.
5. Consumer Directed Health Plans (CDHP) and High Deductible Health Plans (HDHP)
These plans feature high deductibles but allow members to use Health Savings Accounts (HSAs) or Health Reimbursement Arrangements (HRAs) to cover therapy costs. Therapy services are covered but require the deductible to be met first. CDHP and HDHP plans are suitable for providers seeking patients who prefer a lower monthly premium, but reimbursement rates may be delayed until deductibles are satisfied.
6. Catastrophic Plans
Catastrophic plans offer low premiums but high deductibles. They are designed for young adults or those facing financial hardship. Therapy coverage is minimal until the deductible is met, meaning therapy services are generally not reimbursed unless the patient has high healthcare needs.
7. Medicare and Medicaid Plans
BCBS offers Medicare Advantage and Medicaid plans, both of which provide comprehensive therapy coverage. Medicare Advantage plans typically cover outpatient therapy and psychiatric services, with cost-sharing based on Medicare rules.
Medicaid plans provide extensive behavioral health coverage, including therapy services, usually with low or no out-of-pocket costs for those who qualify.
| Plan Type | Network Flexibility | Therapy Coverage Highlights | Cost Considerations |
| Individual & Family Plans | Varies (PPO, HMO options) | Covers mental health, substance abuse, and rehabilitative services per ACA | Premiums vary by metal level; copays/coinsurance apply |
| Group Plans | Typically PPO or HMO | Comprehensive therapy coverage, employer-dependent | Often better negotiated rates and coverage |
| Medicare Advantage | Network-based | Covers outpatient therapy, psychiatric services | Cost-sharing per Medicare rules |
| Medicaid Plans | Network-based | Covers behavioral health, therapy, rehabilitative care | Low or no cost-sharing for eligible individuals |
| PPO | High flexibility | Covers in-network and partial out-of-network therapy | Higher premiums; lower cost-sharing in-network |
| HMO | Restricted to network | Therapy covered in-network only; referral required | Lower premiums; lower out-of-pocket costs |
| CDHP/HDHP | Varies | Therapy covered after deductible; HSA funds can be used | High deductible; tax-advantaged accounts help pay costs |
| Catastrophic | Limited coverage | Therapy coverage limited until deductible met | Low premium, high deductible |
Benefits of Using BCBS Insurance for Mental Health Conditions
Blue Cross Blue Shield insurance offers these valuable advantages for therapy providers.
- Reduces out-of-pocket costs for clients, increasing access to your services
- Expands your client base through BCBS’s extensive network
- Provides reimbursement for various treatment types, including specialized therapies
- Offers flexibility with telehealth and in-person service coverage
- Ensures privacy and compliance, protecting both your practice and client data
FAQs on BCBS Therapy Coverage and Reimbursements
Let us answer a few questions about BCBS therapy reimbursements now.
Do I need to verify patient eligibility for therapy services?
Yes, providers must verify patient eligibility before delivering therapy services. This ensures that the patient’s insurance plan covers the required therapy and that there are no issues with eligibility. To verify, you can use the BCBS provider portal, contact BCBS customer service, or use an eligibility verification system if your practice has one. Always confirm the patient’s benefits to avoid claim rejections.
How do I file a claim for therapy services under BCBS?
To file a claim for therapy services under BCBS, follow these steps:
- Ensure you have the correct CPT codes, dates of service, and diagnosis codes.
- Use the BCBS provider portal for electronic submission or mail the claim to BCBS using the address specified on the provider’s website.
- Track the claim status through the portal or by calling BCBS if needed. Comply with any specific instructions provided by BCBS to avoid delays.
How long does BCBS take to process therapy claims?
On average, BCBS processes therapy claims within 30 to 45 days. However, this time frame can vary depending on several factors, such as claim complexity, network status (in-network or out-of-network), and plan type. You can track the status of claims through the BCBS provider portal for updates.
What should I do if BCBS refuses to pay for therapy services?
If BCBS denies a therapy claim:
- Check the reason provided in the denial notice.
- Call the BCBS provider support line for clarification on the denial and gather more information.
- If you believe the denial was made in error, follow the appeal instructions. This may involve submitting additional documentation to support the claim. Use the correct appeals forms and ensure all required information is provided to avoid further delays.
Does Blue Cross Blue Shield cover therapy services?
Yes, BCBS generally covers therapy services, including individual and group psychotherapy, psychiatric evaluations, and other mental health services. However, coverage can vary based on the patient’s specific plan type, network status, and location. Ensure to check the patient’s plan benefits for details on coverage, limitations, and reimbursement rates.
How do I verify if therapy is covered by a patient’s BCBS plan?
To verify coverage for therapy, check the patient’s Summary of Benefits for the “Outpatient Mental Health” section. You can also use the BCBS provider portal or call BCBS member services to confirm the patient’s therapy benefits, network requirements, and any prior authorization needs.
Can I submit claims for telehealth therapy sessions?
Yes, BCBS covers telehealth therapy, but reimbursement rates may differ from in-person therapy. Providers should use the appropriate telehealth CPT codes (such as 90834 for psychotherapy, 30 minutes) and include the GT modifier to indicate telehealth. Ensure you follow BCBS’s telehealth guidelines and claim submission procedures to ensure timely and accurate reimbursement.
What if the patient chooses an out-of-network therapist with BCBS?
If the patient is seeing an out-of-network therapist, reimbursement will likely be at a lower rate. The patient may be responsible for higher out-of-pocket costs, and you may need to submit a claim for reimbursement if you’re an out-of-network provider. PPO plans typically reimburse some portion of the out-of-network therapy fees, while HMO or EPO plans usually do not reimburse for out-of-network services.
How can I avoid claim denials and ensure correct payment?
To reduce the likelihood of claim denials, follow these best practices:
- Always verify patient eligibility and coverage before delivering services.
- Use accurate CPT, ICD-10, and modifier codes.
- Ensure thorough and complete documentation of each session, including the treatment provided and progress made.
- Submit claims within the required timeframe and use electronic medical billing service whenever possible to speed up processing.
- Regularly track claims status and follow up with BCBS if necessary.




