Patient insurance verification is a complex process. With its significance of automation and ensuring accuracy, it has various challenges and headaches for healthcare providers. They must be aware of how to complete this process successfully. This practical guide is a complete roadmap for healthcare providers to streamline the patient-centric insurance verification process.
Insurance Verification: Provider’s Roadmap
Before starting the insurance verification process, having all the necessary patient and insurance information is essential. Be careful and thorough during this process, as missing or inaccurate information can result in denied claims, due to which practice may face a revenue loss. So, the verification process must be streamlined with accurate patient information.
Here’s what providers should consider before starting the patient insurance verification process.
Patient’s Personal Information
Start with the basics; ensure you have the patient’s full name, date of birth, and contact information. Accurate personal details are essential for a successful insurance verification process.
Policy Holder’s Information
Obtain the full name of the primary insurance policyholder, their relationship to the patient, and, if necessary, their date of birth. This is especially important if the patient is not the primary policyholder.
Insurance Company Details
Gather the insurance company’s name, contact information, and the policy and group number associated with the patient’s plan. This information is needed to contact the insurer to verify the coverage.
Insurance Plan Details
Understand the specifics of the patient’s insurance plan, including the type of plan, coverage details, any exclusions or limitations, and the start and end dates of the policy.
Financial Responsibilities
Confirm the patient’s financial responsibilities under their plan, including copayments, deductibles, and coinsurance. This information is vital to communicate to the patient beforehand to avoid unexpected costs.
Secondary Insurance Information
If the patient has secondary insurance, gather the same information for the secondary insurer. This step is crucial to ensure complete coverage and accurate billing.
Pre-authorization Requirements
Determine if the patient’s plan requires pre-authorizations for any services or procedures. If it does, getting this authorization before providing the services is essential.
Patient Insurance Verification Process
What to Verify?
Healthcare practices and providers must verify various aspects while verifying the insurance eligibility. These include:
- Policy holder name
- Policy effective date
- Policy term date
- Co-pay or coinsurance
- Patient’s deductible and accumulations
- Patient’s out-of-pocket maximum
- Pre-authorization is required or not
How to Verify?
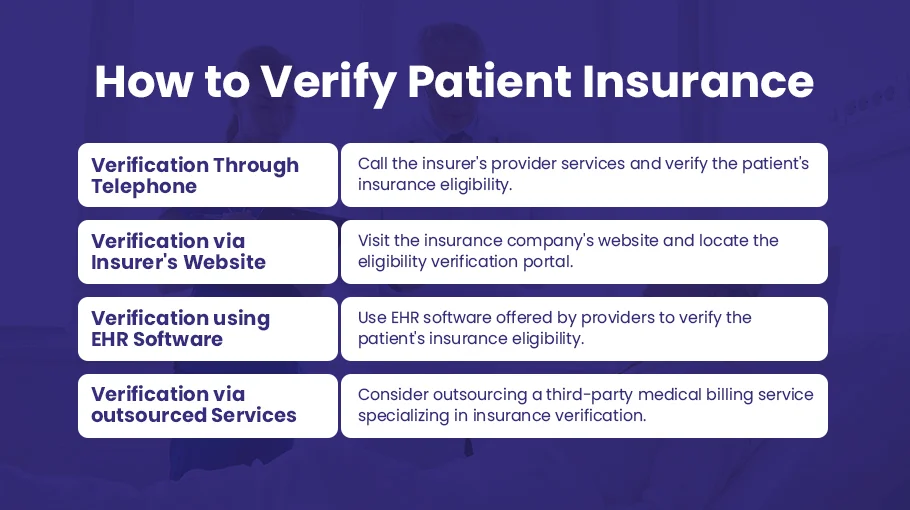
Here are the ways providers can verify the patient’s insurance verification.
1. Telephone Verification:
- Obtain the insurance details from the patient, including their policy number and insurance company contact details.
- Call the insurer’s provider services and verify the patient’s insurance eligibility and benefits.
- Document all vital information, including coverage details, deductible status, copayments, and any requirements for referrals or pre-authorizations.
2. Verification through the Insurer’s Website
- Visit the insurance company’s website and locate their provider services or eligibility verification portal.
- Enter the patient’s policy details and retrieve the eligibility status and benefits information.
- Remember that you’ll need to set up accounts with each insurer, and the details available might vary between insurance companies.
3. Automated Verification using EHR Software
- If your practice uses a practice management system or Electronic Health Record (EHR) system, it might include an insurance eligibility verification feature.
- Input the patient’s insurance details into the system, and it will automatically verify eligibility with the insurance company and retrieve benefit details.
- This method often saves time and reduces administrative workload, but it ensures your software is compatible with the insurers you work with.

4. Outsourcing to a Medical Billing or Verification Service
- Consider outsourcing a third-party medical billing service specializing in insurance verification if your practice has a high patient volume or if you want to free up staff for other tasks.
- Provide the service with your patient roster and insurance details, and they will verify eligibility and benefits on your behalf.
- Although this method involves an additional cost, it might save money in the long run by reducing claim denials and ensuring you collect all the revenue you’re entitled to.

How Bell MedEx Simplifies Patient Insurance Verification Process
Bell MedEx offers a suite of features to simplify and streamline this process for healthcare providers. Here’s how:
Automated Verification Process
Bellmedex integrates EHR software Medifusion, which offers an automated insurance verification feature, allowing providers to instantly check a patient’s insurance status and coverage details. This reduces waiting times and ensures a smoother billing process.
Real-time Access to Data
Having access to real-time insurance information is crucial in the healthcare industry. With Bellmedex, providers can access up-to-date insurance information at any time. This feature reduces time spent communicating with insurance companies and decreases the likelihood of claim denials due to outdated or incorrect information.
Comprehensive View of Insurance Information
Bellmedex offers a comprehensive view of a patient’s insurance details. Providers can easily see the policy status, coverage limits, co-pays, and deductibles, enabling accurate calculation of out-of-pocket expenses. This helps providers to communicate costs with patients, enhancing patient satisfaction transparently.
Secure and Compliant Platform
Security and compliance are paramount in healthcare. Bellmedex ensures that the insurance verification process adheres to all regulations, including HIPAA. Providers can be assured that patient data is secure and that all transactions comply with the law, reducing liability concerns.
Streamlined Workflow
By integrating patient insurance verification into the healthcare provider’s workflow, Bellmedex enhances productivity. The user-friendly interface allows for an easy transition from patient records to insurance verification without switching between systems. This results in a more efficient process, freeing time for healthcare providers to focus on patient care.
Improved Patient Experience
By speeding up and simplifying the insurance verification process, Bellmedex contributes to a better patient experience. Patients receive timely and accurate information about their coverage, leading to fewer cost surprises and more trust in the healthcare provider.
With BellMedEx, go ahead into tomorrow’s healthcare.
Visit our website or contact us to start a journey with us. Find out how we can support your practice by improving your insurance verification process.
Conclusion
Patient insurance verification is a difficult but essential process for healthcare practices. The steps outlined in this guide aid in streamlining this complex process and improving the effectiveness of your practice. Bell MedEx makes the patient insurance verification process easy for practices by providing its practice management system that providers can employ for automated and real-time Verification, preventing errors and streamlining the process.