Medical billing is a crucial process in the healthcare industry. It is submitting and following up on claims with health insurance companies to receive payment for services rendered by healthcare providers. Medical billing involves various activities, from verifying patient insurance eligibility to coding medical procedures accurately. It is essential to have a reliable and efficient medical billing platform to streamline the billing process and improve revenue. This article will discuss how Bell MedEx can help healthcare providers improve their billing processes effectively.
How Bellmedex Improves Billing Process?
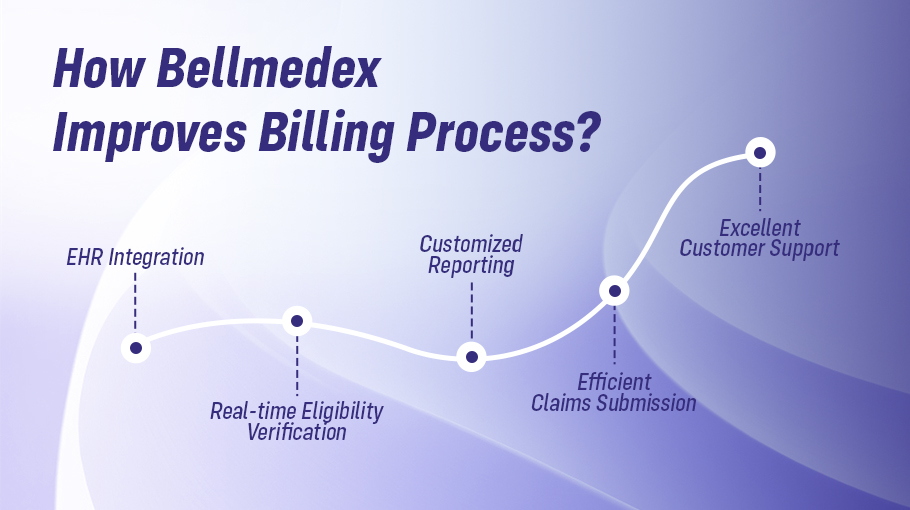
Bell MedEx is a comprehensive medical billing platform designed to help healthcare providers manage their billing processes efficiently. It offers a range of features to streamline the billing process and reduce errors, including real-time eligibility verification, EHR integration, effective claims submission, and customized reporting.
EHR Integration
Electronic Health Records (EHR) are becoming increasingly popular in healthcare facilities as they offer a range of benefits, such as improved patient care and reduced paperwork. Bell MedEx integrates seamlessly with EHR systems like Medifusion, allowing healthcare providers to quickly transfer patient information from the EHR to the billing platform. This eliminates the need for manual data entry, reducing the risk of errors and saving time.
Real-time Eligibility Verification
Verifying patient insurance eligibility is a crucial step in the medical billing process. Without verifying insurance eligibility, healthcare providers risk submitting claims that will be denied, resulting in a loss of revenue. Bell MedEx offers real-time eligibility verification, which allows healthcare providers to verify a patient’s eligibility for insurance coverage in real-time. This reduces the risk of claim denials and ensures that healthcare providers are reimbursed for their services.
Customized Reporting
Customized reporting is essential in medical billing platforms, allowing healthcare providers to monitor billing processes and revenue. With Bell MedEx, healthcare providers can create customized reports that provide insights into their billing processes. These reports can help healthcare providers identify areas for improvement and make data-driven decisions to improve their billing processes.
Efficient Claims Submission
Efficient denial management requires clean claim submission. Complete data collection, accurate coding, and appropriate billing are necessary for a clean claim clearance. Clean claims that are initially submitted aid in quickly recovering the costs. Bell MedEx helps providers to submit claims successfully with a proper follow-up process. This allows practices to track and record the claim processing phases.
Excellent Customer Support
Bell MedEx offers excellent customer support to healthcare providers. With a team of knowledgeable and friendly support staff, healthcare providers can get the help they need to manage their billing processes effectively. Bellmedex’s support team can answer questions and guide you on using the platform’s features.
Conclusion
Medical billing is a critical process that requires a reliable and efficient platform. Bellmedex offers healthcare providers a comprehensive platform to manage billing processes, streamline workflows, and improve revenue. With its features and excellent customer support, Bell MedEx is a great choice for healthcare providers looking to improve their billing processes. By using Bell MedEx, healthcare providers can reduce errors, save time, and improve revenue.