According to the American Diabetes Association (ADA), approximately 8.4 million U.S. residents rely on insulin to manage their blood sugar and diabetes. With such a significant number, it is clear to healthcare providers that ensuring patients have affordable access to diabetes treatment is crucial.
However, securing Medicare coverage for insulin and related supplies, like needles and syringes, can be difficult for healthcare providers.
Medicare covers insulin and related supplies under specific conditions that healthcare providers must understand. These complexities can lead to confusion and unexpected patient costs if not handled correctly.
If you’re unsure whether Medicare covers insulin needles, you’re in the right place. In this blog, we will clarify whether Medicare covers insulin needles.
💡 Do you know:
Insulin is a hormone that regulates blood sugar (glucose) levels. It is produced by the beta cells in the islets of Langerhans in the pancreas.
Medicare Insurance Plans
Before determining whether Medicare covers insulin needles, healthcare providers must understand the insurance plans offered by Medicare.
Medicare, the federal health insurance program primarily for individuals aged 65 or older, is divided into different parts, each covering various healthcare services:
- Medicare Part A (Hospital Insurance): Covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care.
- Medicare Part B (Medical Insurance): Covers outpatient care, doctor services, and certain preventive services.
- Medicare Part C (Medicare Advantage Plans): Offered by private companies approved by Medicare, these plans include Part A, Part B, and sometimes Part D.
- Medicare Part D (Prescription Drug Coverage): Helps cover the cost of prescription drugs.
Coverage becomes more nuanced when it comes to insulin and related supplies, like insulin needles. Providers need to understand the specifics of both Part B and Part D for proper coverage. Many providers remain confused about whether insulin needles are covered, so it’s crucial to understand how Medicare addresses this.
Does Medicare Cover Insulin Needles?
Yes, Medicare covers insulin, but it depends on how you administer it.
Let’s break this down:
➜ Medicare Part B covers insulin if you use an insulin pump, which is considered durable medical equipment. However, it does not cover insulin pens or supplies like syringes, needles, alcohol swabs, or gauze.
➜ Medicare Part D covers insulin that is not used with a traditional insulin pump, along with certain medical supplies needed to inject insulin, such as syringes and needles. The cost for a one-month supply of each covered insulin product is capped at $352.
➜ Medicare Part D covers insulin needles, Medicare Part B does not. However, if you have a Medicare supplement insurance plan that covers your Part B coinsurance, it may help pay for insulin under Part B.
| Medicare launched a Part D Senior Savings Model in 2021 to offer insulin at a maximum copayment of $35 for a month’s supply. However, not all prescription drug plans are part of this model. Individuals can review what available plans offer using Medicare’s search tool. |
When covering insulin and related supplies, understanding the distinctions between Part B and Part D is crucial for providers.
Now, let’s explore these differences in more detail:
When a Patient Has a Medicare Part B Plan
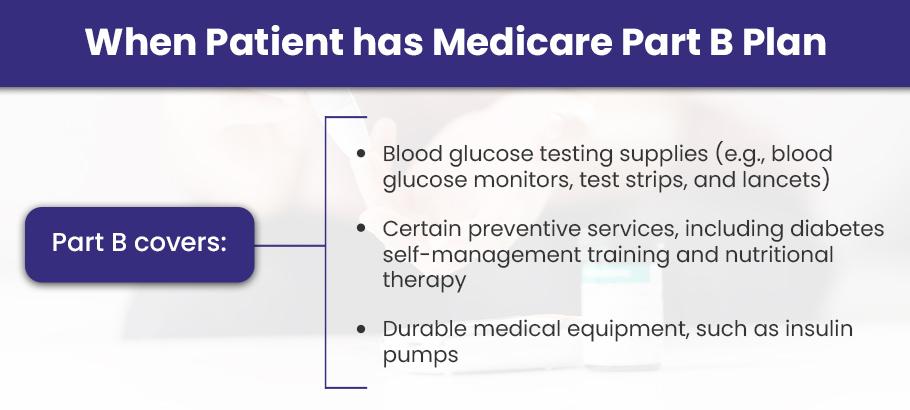
Medicare Part B is a component of Medicare that covers medical services and supplies necessary for treating or managing health conditions.
Medicare Part B covers a variety of services and supplies, such as:
- Blood glucose testing supplies (e.g., blood glucose monitors, test strips, and lancets)
- Certain preventive services, including diabetes self-management training and nutritional therapy
- Durable medical equipment, such as insulin pumps
- Therapeutic shoes or inserts
However, Medicare Part B does not cover the following diabetes-related supplies:
- Insulin pens
- Syringes
- Needles
- Gauze
- Alcohol swabs
So, to answer your question: Medicare does not cover insulin needles under Part B.
It’s important to remember that Medicare Part B covers insulin when administered via an insulin pump that qualifies as durable medical equipment (DME). This coverage can be a significant benefit for patients who need continuous insulin infusion through a pump, as both the pump and the insulin used in it may be covered.
However, while Part B covers the insulin and the pump, it generally does not cover needles or syringes for manual insulin administration.
REMEMBER:
➜ The doctor should include insulin for the Durable Insulin Pump. For example, for a patient using a Medtronic durable pump, the doctor’s order should consist of “Insulin for Durable Insulin Pump.”
➜ When billing Medicare for insulin administered through a pump, ensure compliance using HCPCS codes such as J1815 (injection, insulin, per 5 units) and DME billing codes.
➜ Always verify that the patient’s specific insulin pump qualifies under Medicare’s list of durable medical equipment to avoid claim denials.
Under the Part B plan, patients are responsible for paying 20% of the cost in 2024, while Medicare covers the remaining 80%. These costs are in addition to other out-of-pocket payments for Part B, including the monthly premium, yearly deductible, and copayments.
When the Patient Has a Medicare Part D Plan
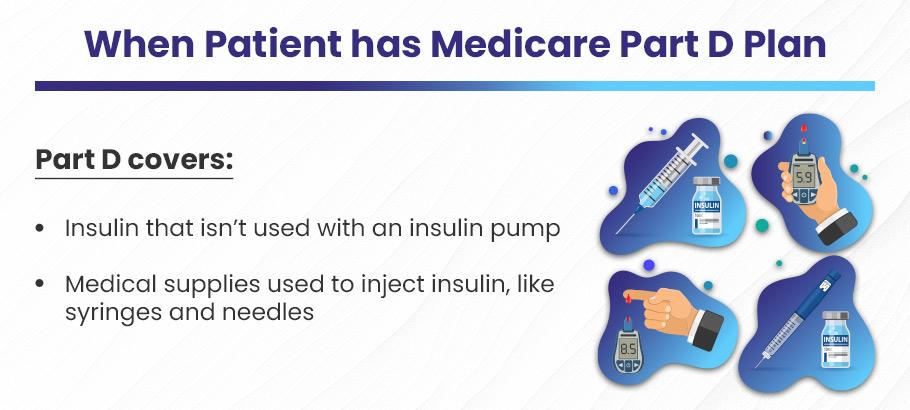
Medicare Part D is the prescription drug plan that covers medications and certain medical supplies needed to administer them.
Patients need a Part D plan for insulin and related supplies, such as needles and syringes. Here’s what Part D covers:
- Insulin that isn’t used with an insulin pump
- Medical supplies used to inject insulin, like syringes and needles
Part D plans also cover a one-month supply of each covered insulin product, with a capped cost of $35.
| Key Consideration for Providers: Patients who rely on self-injections or pens must ensure that their Part D plan includes coverage for these items. Providers should guide patients through reviewing their plan’s formulary to confirm that the required needles and other supplies are covered. |
Medicare Part D, which provides prescription drug coverage, typically includes the cost of insulin and the supplies needed to inject it—such as needles, syringes, alcohol swabs, and gauze. This is especially important for patients who self-administer insulin, as it ensures they have access to both the medication and the necessary tools to use it effectively.
When your patient has a standalone Part D plan or a Medicare Advantage plan that includes drug coverage, you must verify that their specific plan covers these supplies. Each Part D plan has a formulary—a list of covered drugs and supplies—which can vary by plan.
As a provider, it’s essential to confirm the coverage beforehand to avoid surprises at the pharmacy, where patients may otherwise face unexpected out-of-pocket costs.
Before proceeding with billing and claim submission, make sure that the pharmacy providing these drugs and supplies is in-network.
The Medicare Pricing Plan for Diabetes
As a healthcare provider, you must be aware of the costs of insulin that Medicare charges. Below is the breakdown of three plans for Medicare insulin costs.
Medicare Insulin Costs
1). Insulin Under Part D (Prescription Drug Plan):
- You’ll pay no more than $35 for a one-month supply of insulin covered by your Part D plan.
- If you get a 3-month supply, your total cost will be capped at $105 ($35 per month).
- If you receive Extra Help, your costs will be even lower.
2). Disposable Insulin Patch Pumps:
- Insulin for disposable patch pumps is covered under your Part D plan, with a maximum cost of $35 per month.
- The insulin patch pump itself, if covered, may cost more than $35, as it is not considered an insulin product.
3). Insulin Covered by Part B (Durable Medical Equipment):
- If you use an insulin pump covered by Medicare Part B or a Medicare Advantage Plan, your monthly insulin costs will be capped at $35.
- If you have Medigap insurance to cover Part B coinsurance, it should cover the $35 insulin cost.
For more information:
- Visit Medicare.gov/coverage/insulin.
- Call 1-800-MEDICARE (1-800-633-4227), TTY 1-877-486-2048.
FAQs
1). Are pen needles covered by Medicare?
Yes, Medicare covers pen needles. Providers are reimbursed for the pen needles under the Medicare Part D plan. Pen needles are used by providers to treat asthma attacks and severe allergic reactions. Pen needles from various brands covered by Medicare include:
- Auvi-Q
- EpiPen
- EpiPen 2-Pak
- EPIsnap
- Adyphren
- EpinephrineSnap-V
- Bronchial Mist Refill
- Adyphren II, Adyphren Amp II
- Adyphren Amp
2). What insulin is covered by Medicare?
Medicare covers insulin used with a disposable or non-traditional insulin pump, not an insulin pump itself. Medical supplies used to inject insulin include syringes, gauze, and alcohol swabs.
3). What insulin is covered by Medicare Part B?
Medicare Part B covers insulin used with an insulin pump, as part of the durable medical equipment benefit. Remember, Part B does not cover insulin pens or insulin-related supplies like syringes.
4). What insulin is covered by Medicare Part D?
Medicare Part D (also called the Drug Coverage Plan) covers insulin used with injectables like syringes or pens. However, it does not cover insulin used with a disposable or non-traditional insulin pump.
Final Thoughts
Medicare Part D typically covers the supplies needed to inject insulin, including needles, syringes, alcohol swabs, and gauze. However, Part B can come into play when insulin is administered through an insulin pump.
In conclusion, we can say that Medicare covers the Insulin needles but only under its Part D plan.
So, to successfully reimburse the treatments given to your patient with diabetes, confirm that they have a Medicare Part D Plan.