Prior authorization can be quite frustrating and time-consuming, especially for medications! But it ensures that the prescribed medication is medically necessary, appropriate for the patient’s condition, and cost-effective.
The good news is that there are ways to expedite the process. And this guide covers 13 proven tips to speed up prior authorization for medication. We’ll also answer some questions about prior auth. for medications.
Making Sense of Prior Authorization for Medication
Prior authorization (PA) for medication is a process in which healthcare providers get approval from a patient’s insurance company before prescribing certain medications. This approval is usually required for expensive drugs, those with a higher potential for misuse, or medications that have lower-cost alternatives.
How to Obtain a Speedy Prior Authorization for Medication
Healthcare providers must obtain prior approval from payers for specific medications. For that, they must check the patient eligibility, medical necessity, complete the prior authorization form, and submit it to the insurance.
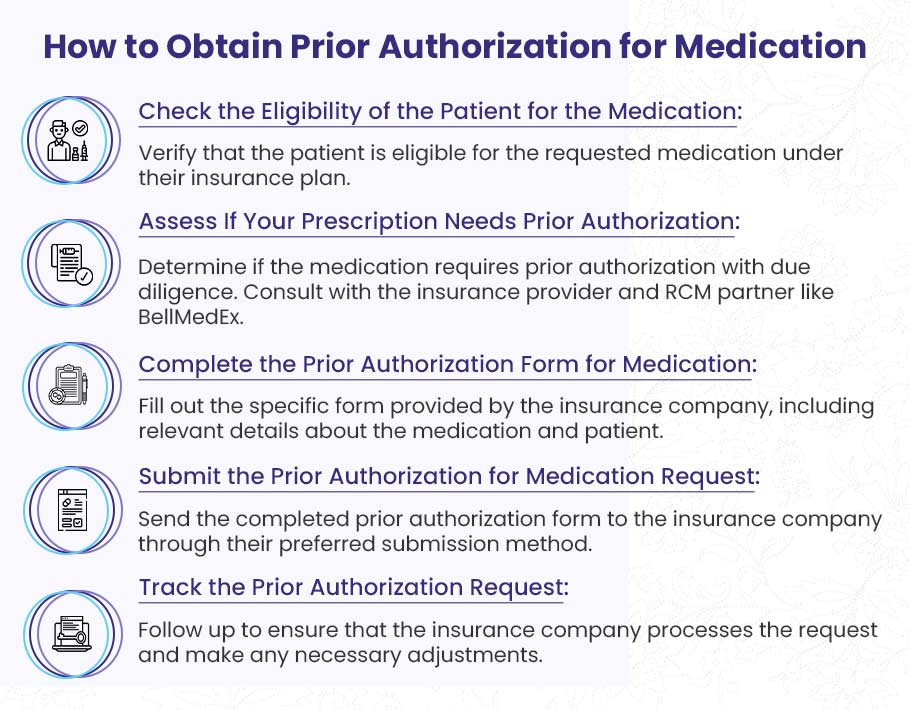
➜ Check the Eligibility of the Patient for the Medication: Verify that the patient is eligible for the requested medication under their insurance plan.
➜ Assess If Your Prescription Needs Prior Authorization: Determine if the medication requires prior authorization with due diligence. You can also consult with the insurance provider and RCM partner like BellMedEx.
➜ Complete the Prior Authorization Form for Medication: Fill out the specific form provided by the insurance company, including relevant details about the medication and patient.
➜ Submit the Prior Authorization for Medication Request: Send the completed form to the insurance company through their preferred submission method.
➜ Track the Prior Authorization Request: Follow up to ensure that the insurance company processes the request and make any necessary adjustments.
Despite these clear steps, you may face many challenges during the prior authorization process, depending on varying payer requirements, constantly changing rules, and a lack of transparency.
6 Common Challenges in the Prior Authorization Process
These challenges can lead to delays. That’s why, we must understand them quickly before we jump into speeding up the process.
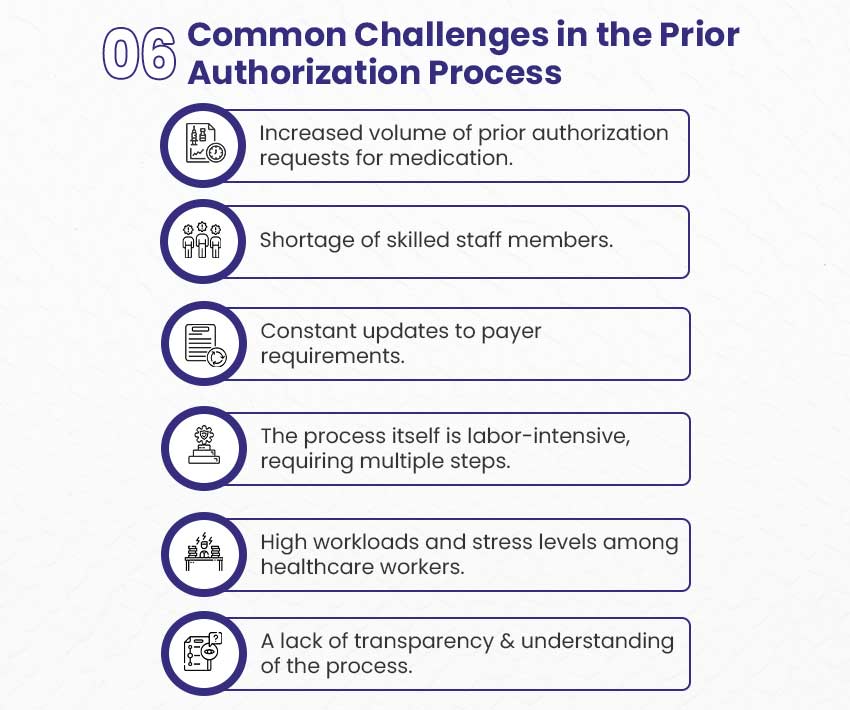
- Increased volume of prior authorization requests for medication.
- Shortage of skilled staff members.
- Constant updates to payer requirements.
- The process itself is labor-intensive, requiring multiple steps.
- High workloads and stress levels among healthcare workers.
- A lack of transparency and understanding of the process.
Let us now jump on the ways to tackle these challenges and expedite medication prior authorization.
⬇️⬇️⬇️
How to Speed Up Prior Authorization for Medication
Speeding up the prior authorization process for medication helps ensure that patients receive timely care. Reduced delays help healthcare providers improve patient outcomes, reduce administrative burdens, and increase practice efficiency.
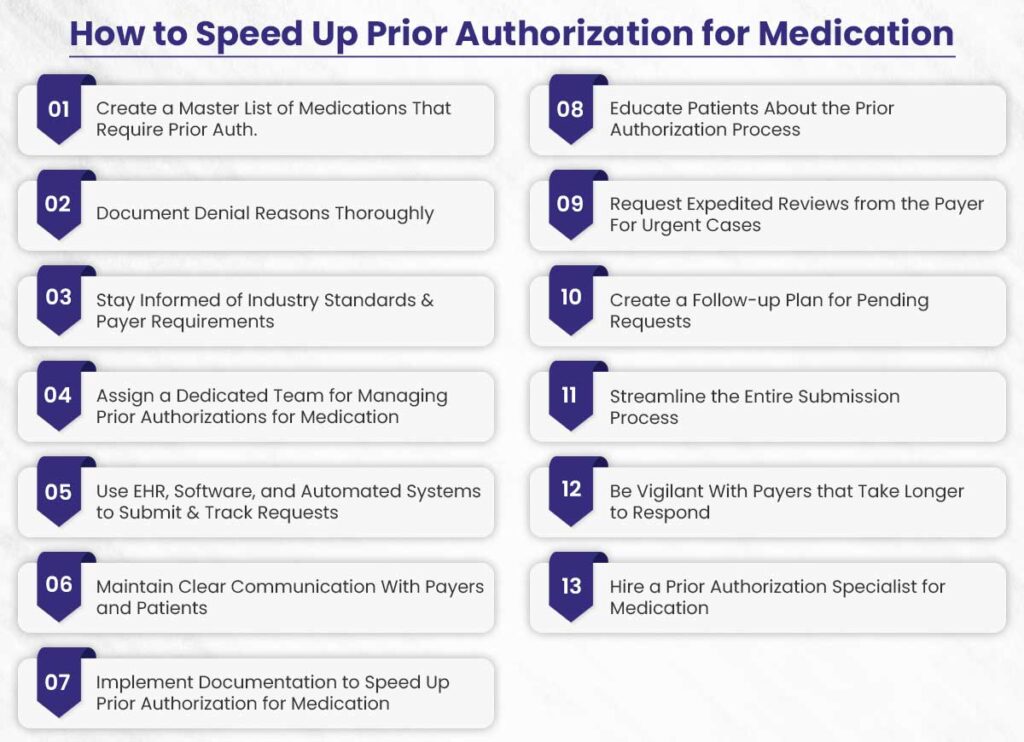
These are 13 practical tips to accelerate prior authorization for medication:
- Create a Master List of Medications That Require Prior Authorization
- Document Denial Reasons Thoroughly
- Stay Informed of Industry Standards & Payer Requirements
- Assign a Dedicated Team for Managing Prior Authorizations for Medication
- Use EHR, Software, and Automated Systems to Submit & Track Requests
- Maintain Clear Communication With Payers and Patients
- Implement Documentation to Speed Up Prior Authorization for Medication
- Educate Patients About the Prior Authorization Process
- Request Expedited Reviews from the Payer For Urgent Cases
- Create a Follow-up Plan for Pending Requests
- Streamline the Entire Submission Process
- Be Vigilant With Payers that Take Longer to Respond
- Hire a Prior Authorization Specialist for Medication
Let us understand each method in a little detail now.
1. Create a Master List of Medications That Require Prior Authorization
Creating a master list of medications that require prior authorization helps streamline the process. Keeping this list organized and up-to-date helps healthcare providers quickly determine which medications need prior approval before prescribing them.
This proactive approach helps reduce delays, as providers can verify authorization requirements ahead of time and avoid unnecessary back-and-forth with insurance companies. Payers provide you this list, but you should be constantly checking it for updates. Also, ensure all staff members know this list well to avoid missing approvals and help patients get care faster.
2. Document Denial Reasons Thoroughly
Thoroughly documenting the reasons for prior authorization denials for medication helps prevent repeat issues. When a request is denied, record the specific reason given by the payer, including any missing information or required documentation.
This helps healthcare providers understand common issues that may lead to denials and make necessary improvements for future requests. Recording the reasons for denials helps when challenging decisions, as it clearly shows why the request was turned down.
3. Stay Informed of Industry Standards & Payer Requirements
The prior authorization for medication can vary greatly between different insurance companies and over time. Staying informed about industry standards and changes to payer requirements is important for smooth processing.
Regularly review payer guidelines, participate in industry webinars, and subscribe to payer newsletters to ensure you’re always up-to-date on the latest changes.
4. Assign a Dedicated Team for Managing Prior Authorizations for Medication
Assigning a dedicated team to handle prior authorizations for medication can speed up the process. When a specific team or staff member is solely responsible for this task, they become more familiar with payer requirements and can address issues quickly.
Specialization helps improve efficiency as the team gains expertise in navigating the complexities of prior authorizations. This approach also helps prevent burnout and ensure that the medication approvals are smooth.
5. Use EHR, Software, and Automated Systems to Submit & Track Requests
Leverage technology to speed up the prior authorization process for medication. Electronic Health Records (EHR), specialized software, and automated systems can streamline the submission and tracking of prior authorization requests.
These tech stacks allow for quicker submission, better organization of patient data, and real-time tracking of the approval status. Automated systems can also send reminders for follow-ups, reducing the chances of missed deadlines or duplicate submissions.
6. Maintain Clear Communication With Payers and Patients
Clear communication with both payers and patients is one of the best ways to speed up the prior authorization, especially for medication. When submitting a request, ensure that all required documentation is included and provide any additional information promptly if requested by the payer.
Also, keeping patients informed about the status of their authorization and any potential delays helps manage their expectations and reduces frustration. Regular, transparent communication ensures positive relationships with both parties.
7. Implement Documentation to Speed Up Prior Authorization for Medication
Effective documentation ensures that prior authorizations for medication are efficient. Ensure that clinical data, including diagnosis codes, medical history, and rationale for prescribing a specific medication, is well-documented and up-to-date.
Having this information readily available helps prevent delays due to missing or unclear documentation. Well-organized and detailed documentation makes the process smoother for both healthcare providers and payers, reducing the risk of rejections or the need for resubmission.
8. Educate Patients About the Prior Authorization Process
Educating patients about the prior authorization, especially for medication, helps set realistic expectations and reduce their frustration. Many patients are unaware of the complexities and time involved in securing prior authorization.
And this can lead to confusion and dissatisfaction. Educating them about the process and potential delays ensure you’re on the same page. This transparency also creates a long-term relationship between you and patients.
9. Request Expedited Reviews from the Payer for Urgent Cases
Healthcare providers must request an expedited review to speed up the prior authorization for urgent medication cases. If a patient’s condition requires immediate attention, healthcare providers must contact the payer to address the issue.
Payers often have protocols for handling urgent requests, which can help accelerate the approval process. By the way, prior authorization is not required for emergency cases.
10. Create a Follow-up Plan for Pending Requests
Having a follow-up plan in place for pending prior authorization requests for medication ensures timely approvals. Regularly checking on the status of pending requests can identify any issues early on, allowing you to address them before they result in delays.
A systematic follow-up plan, such as following up every 24-48-72 hours, ensures that no request slips through the cracks. It also allows healthcare providers to stay informed about the progress of the authorization process.
11. Streamline the Submission Process
Streamline the submission process for medicinal prior authorizations to reduce delays. You can use standardized forms, ensure all necessary documentation is attached, and submit requests through electronic portals when available.
A streamlined process minimizes the chance of errors, missing information, or incomplete submissions that could delay approval. The more organized and consistent the submission process is, the quicker the authorization will be processed, ultimately leading to faster patient care.
12. Be Vigilant With Payers That Take Longer to Respond
Some payers may take longer to respond to prior authorization requests for medication. Be vigilant when working with these payers and proactively follow up on any delays.
Track the response times of various payers to identify which ones tend to take longer and take extra measures to expedite the process. This vigilance ensures that no request is forgotten, and that providers can address delays even before time.
13. Hire a Prior Authorization Specialist for Medication
Hiring a dedicated prior authorization specialist for medication is a proven way to speed up the process. A specialist with experience in handling prior authorizations for medication can manage the complexities of insurance requirements efficiently.
And that’s where BellMedEx comes in to help you track requests, resolve issues, and communicate effectively with both payers and patients. We ensure swift prior authorization for medication to reduce the administrative burden on your staff.
FAQs About Speeding Up Prior Authorization for Medication
In case we didn’t answer your question, you can contact us right away.
How long does prior authorization take for medication?
Most medication prior authorizations take 2-3 days, but this can change depending on the medicine type and insurance company. Some urgent requests might be approved within hours. For exact timing, it’s best to ask your insurance company directly.
How to check on a prior authorization for medication?
You can check your prior authorization status by calling your insurance company, checking their website or using their online portal (if available). The time it takes to receive a decision can vary depending on the insurer’s workload and internal processes. Regular follow-up helps you stay informed and fix any problems quickly.
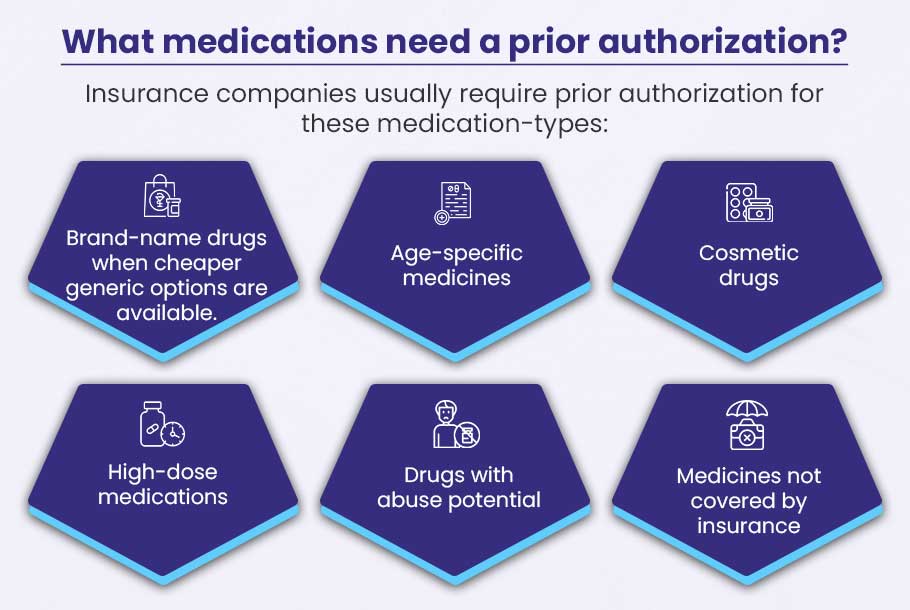
What medications need a prior authorization?
Insurance companies usually require prior authorization for these medication-types:
- Brand-name drugs when cheaper generic options are available
- Age-specific medicines
- Cosmetic drugs
- High-dose medications
- Drugs with abuse potential
- Medicines not covered by insurance
Note: You can get the exact list of medication requiring prior authorization from your payers.
Prior authorization for medication denied, what to do now?
Follow these steps if prior authorization for medication is denied:
- Find out why it was denied
- Check for simple mistakes like wrong codes or spelling
- Ask your doctor to provide more information if needed
- Submit a new request or appeal the decision
- Work with your doctor and insurance company to fix the issue
Speed Up Prior Authorization for Medication With BellMedEx
We can make your prior authorization process smoother and faster. Schedule a free consultation with us to learn how we can help your practice reduce denials and streamline your authorization workflow.