Getting healthcare reimbursement is not like conventional trade to pay and get services, or provide services and get paid. It involves a complete process of registering patients, providing care services, preparing and submitting claims, and getting reimbursed by the insurance providers or patients.
This whole process may take a month long or sometimes longer. Due to many reasons i.e. incorrect claims submission, patient illegibility, non-covered services, etc. claims get denied, and healthcare providers have to wait long summers for reimbursements.
However, if your claim is denied…
You don’t need to launch a thousand ships to get reimbursements after providing healthcare services.
Get medical reimbursement services while outsourcing a full-service medical billing company at a lesser budget than you spend on your in-house team; and get paid on time for the healthcare services you have provided… Yeah, it’s that simple!
This comprehensive guide will help you understand everything about medical reimbursement and the importance of medical reimbursement services.
What is Healthcare Reimbursement?
Medical reimbursement or healthcare reimbursement is the term used for the “money” healthcare providers, diagnostic centers or clinics receive from Government (Medicaid and Medicare) or private insurance companies, or from patients for the medical services they have provided. These care services include all treatment services medically necessary ranging from routine checkups, diagnosis to surgical procedure and long-term care.
Furthermore, in some cases the insurance providers (both govt. and private) may not pay the full amount of healthcare services the patients receive. Then, in-network patients have to pay some portion of the amount known as copayment and co-insurance. On the other hand, the patients have to pay all the cost of care out of their own pocket (self-pay) in case they are not part of insurers’ network.
Do you know?
Approximately, 8% of the US population are not part of any health insurance, and pay out of pocket for the medical services they receive.
Here’s a list of the different healthcare provider payment systems:
➜ Copayment
Copayment is a fixed amount patient pay providers for healthcare services they receive as private insurers or government payers may not pay for the entire cost of a covered service.
➜ Coinsurance
Coinsurance, on the other hand, is the percentage of cost patients pay providers after they have met their annual deductibles.
➜ Self-Pay
Self-pay when patients have no insurance coverage and have to pay providers out of pocket for healthcare services they receive.
➜ Balance Billing
Balance billing or surprise billing is the difference in the provider’s charged amount and the allowed amount. It involves bills from providers to patients for the services they have provided. For example, the cost of the services patients receive is $120, but the allowed amount is $90. The patients will receive a surprise balance bill for the remaining $30.
Types of Reimbursements in Healthcare
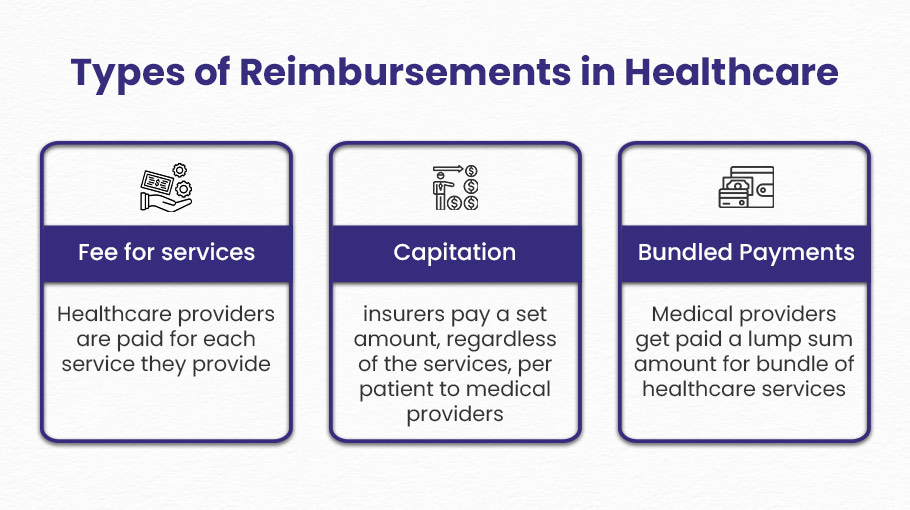
There are three main models of reimbursement in healthcare:
Fee for Services
Fee for services is the most common method or type of reimbursement. Under this method, patients or insurers pay the healthcare providers for each service provided i.e. a doctor’s visit, test, or procedure. The Fee-for-services model facilitates healthcare providers to deliver more and more care services because the reimbursement is not based on quality but quantity of care.
However, this model is not much appreciated as it can lead to overutilization of care services just to get high reimbursements.
Capitation
Capitation is a model of reimbursement in which insurers pay a set amount, regardless of the services, per patient to medical providers for a specific period i.e. a month or a year to ensure quality healthcare treatment.
As per this reimbursement model, the provider is responsible to care for that specific patient within the set time period. The insurance providers encourage healthcare providers to provide quality treatment to patients and keep them healthy to minimize the need for costly treatment procedures. This reduces the treatment expenses and improves the quality of care. Capitation reimbursement method is used in managed healthcare plans i.e. HMOs (health insurance plan that limits coverage to a network of healthcare providers).
The capitation method, however, is advantageous for providing quality healthcare but it may not provide proper compensation for specialized care services.
For example, think about a patient who has a long-term illness. This patient needs to see doctors often and get special treatments. In a capitation model, the healthcare provider gets a fixed payment for each patient. This payment might not be enough to pay for more expensive care, like specialist visits, tests, and long-term treatment of the illness. As a result, providers might be encouraged to reduce referrals or important tests to keep costs down. This could affect the quality of care for patients who need more serious treatment. This imbalance shows a main problem with the capitation reimbursement model: it helps with general health care, but it might not handle the complicated and expensive needs of specialized healthcare well.
Bundled Payments
Bundled payment is a novel form of remuneration in healthcare where providers receive a single aggregated payment amount covering the total anticipated costs for a grouped set of medical services for a patient over an episode of care. The aim is improved efficiency and quality. This consolidated reimbursement model for a bundle of services often relates to a single treatment, like a surgery or rehabilitation stay. Payment depends on both service excellence and thrift. For example, one bundled payment could cover all physician, hospital, and rehabilitation services for a joint replacement patient.
What are Medical Reimbursement Services?
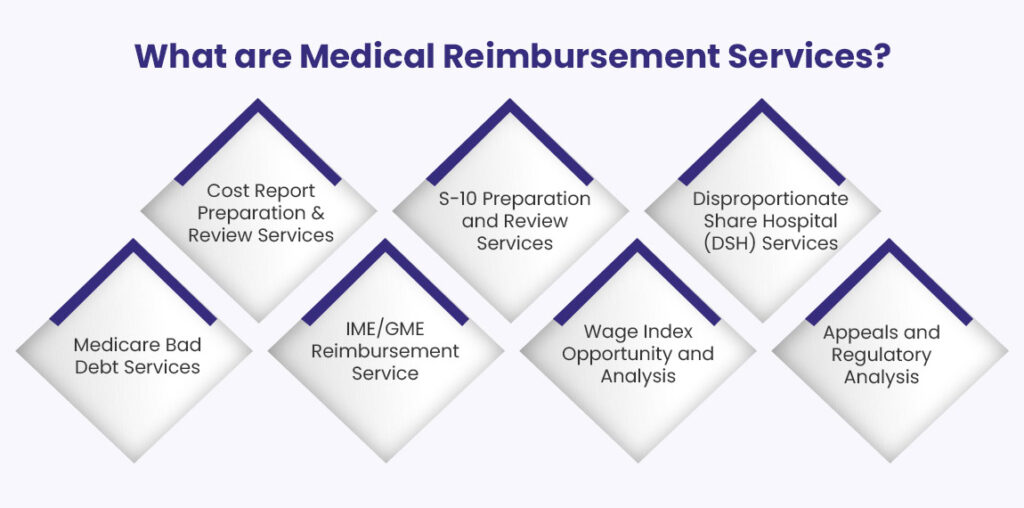
Medical reimbursement services are comprehensive services provided by a third party to healthcare providers helping them get paid timely and maximize healthcare reimbursement rates. These third-party organizations are known as full-service medical billing companies. The healthcare reimbursement services provided by an outsourced medical billing company include:
- Cost Report Preparation and Review Services
- S-10 Preparation and Review Services
- Disproportionate Share Hospital (DSH) Services
- Medicare Bad Debt Services
- IME/GME Reimbursement Service
- Wage Index Opportunity and Analysis
- Appeals & Regulatory Analysis
1). Cost Report Preparation and Review
Cost report preparation and review services are critical tools for healthcare providers to maximize reimbursements. Medical billing companies offer end-to-end support with these complex processes.
Cost reports contain detailed financial and statistical data, such as facility information, costs and charges by department, and Medicare charges. Billing companies help providers compile accurate reports that comply with the latest regulations, leveraging their medical reimbursement services to ensure compliance. Their experts analyze the data to identify opportunities to improve financial performance and reimbursement rates.
For example, they may find areas where coding can be optimized or expenses reduced through their medical reimbursement solutions. They also assist with preparing required supporting documents, making the cost report preparation process more efficient. Thorough reports and compliance help providers avoid penalties and audits.
In addition to preparation, billing companies offer cost report review services as part of their healthcare reimbursement solution. If a provider prepares an in-house report, the billing experts still review it prior to submission. They identify any issues or errors and recommend improvements for completeness and accuracy. Their objective, through these medical reimbursement services, is to ensure the reports maximize appropriate reimbursements.
2). S-10 Preparation and Review
Preparing and reviewing cost reports is important for healthcare providers who want to get the most money back, especially from Medicare. The S-10 worksheet is very important in this process. It is used to report costs and to document charity care and uncompensated care. Filling out the S-10 correctly is very important because it affects how much money a provider gets from Medicare and Medicaid.
The S-10 worksheet needs clear financial information. This includes how many patients do not have insurance and the costs for their treatment. This information helps Medicare adjust how much money hospitals get paid. It shows how much it costs to care for people who do not have insurance. Medical billing companies help providers by preparing the S-10 worksheet through their Medical Reimbursement Services.
These companies help you from start to finish in creating correct cost reports. They make sure to follow the latest rules from the Centers for Medicare & Medicaid Services (CMS). Their experts look at the data in the S-10 to find ways to improve financial performance and increase reimbursement rates. For example, they can assist healthcare providers in correctly recording and reporting charity care, making sure they get the right payment for the services they provide.
Also, medical reimbursement services help prepare the necessary documents, making the cost report more reliable. Well-documented reports make it easier to get paid back and help providers stay away from expensive fines and checks.
In addition, third party medical billing companies help by reviewing cost reports. Even if a provider makes an S-10 report themselves, billing experts will check it before sending it in, finding any possible problems or mistakes. They give suggestions to make things better, making sure the report is full and correct. The main aim of these medical reimbursement services is to get the right payments. This helps healthcare providers keep running their services and offer good care to patients.
By using the skills of medical billing companies to handle S-10 worksheets and cost report preparation, healthcare providers can improve their financial results and follow Medicare rules.
3). Disproportionate Share Hospital (DSH)
According to federal law, Medicaid provides Disproportionate Share Hospital (DSH) payments to hospitals that serve a large number of Medicaid and uninsured patients. These payments are important for helping hospitals pay for the care of patients who might not be able to afford it. For instance, a hospital in a low-income area that helps many uninsured people can get DSH funding to help with the costs of those services.
Medical reimbursement service from a medical billing company helps hospitals get better funding from DSH. They make sure that all important documents are ready and sent in the right way, increasing the chances of getting these important payments. By getting DSH payments, healthcare practices can raise their total income. This helps them stay financially healthy and keep serving their communities well.
4). Medicare Bad Debt
Medicare bad debt is a term used for the amount that Medicare beneficiaries owe to a healthcare provider for deductibles and coinsurance; and the provider is unable to collect. After reporting on the cost report, Medicare reimburses providers with 65% of the allowable bad debt. Healthcare practices need to be in partnership with outsourced medical billing companies to get reimbursed as much as possible for the services they have provided to Medicare patients who are unable to pay their dues. These billing companies also reduce stress from healthcare providers by providing them with comprehensive services fulfilling all the requirements and performing potential audits.
5). IME/GME Reimbursement
Getting the right money back for residency training expenses is very important for healthcare providers, but the IME and GME programs can be hard to understand by themselves. Working with a skilled medical billing company for reimbursement services helps providers get all the money they deserve to get for the important training of future doctors.
Outsourcing the reimbursement process helps providers concentrate on giving great training, while expert billing staff take care of the details for Medicare cost preparation and reporting. Experienced billing teams know the qualifications and documents needed to get the most money back for indirect costs, like administrative expenses, and for direct costs related to graduate medical education programs by Medicare i.e Indirect Medical Education (IME) and Graduate Medical Education (GME). They are skilled in cost identification, cost allocation, cost apportionment, and cost finding results in accurate reimbursement.
Providers can trust that their residency programs will be funded correctly by using the knowledge of third party billing experts. The reimbursement specialists help reduce paperwork, allowing providers to spend more time mentoring residents. Their work to get every reimbursement dollar helps ensure financial stability. This allows them to keep providing high-quality training that will shape the future of healthcare.
6). Wage Index Opportunity and Analysis
Many factors affect how much providers are paid for their services. One such important component is the Wage Index. It is a metric that measures the relative hospital wage level in a geographic area compared to the national average. This has a direct impact on the payment rates set by CMS for providers. As such, healthcare organizations need to be careful when gathering and sharing wage data. This helps make sure the wage index shows their labor costs correctly and gets them the most money back.
This is where outsourced medical billing services show their benefits. Medical billing companies help clients understand wage index opportunities in detail. This means carefully looking at current pay data and forecasts to find any mistakes or problems that could hurt payments. The billing team works with the healthcare provider to fix the wage data and make sure the reports to CMS and other payers are correct.
Managing wage indexes actively is very important for the financial health and long-term success of healthcare providers.
Also, outsourced billing experts keep an eye on changes in wage index rules and trends. They inform clients about any changes that might create risks or chances for reimbursement. Their knowledge and careful attention to wage index details can greatly affect payments for healthcare providers. This helps the provider organization focus on giving good care while relying on the billing partner to improve revenue and payments.
7). Appeals & Regulatory Analysis
Appeals and regulatory analysis are important services provided by medical billing companies to ensure timely and accurate reimbursement for healthcare providers. Healthcare rules and insurance needs can be complicated, so it is common for claims to be denied. Billing companies hire experts to help with appeals and to solve these denials.
A good appeals process is important for getting back denied claims and lost money. When a claim is denied, billing specialists look into why it happened, gather documents to support the services, and send a clear appeal according to the rules of the payer. They are very skilled in medical coding and compliance, which helps them win many appeals. Regulatory analysts regularly check new rules to make sure billing and documentation follow the requirements. They look for ways to get the most money back while following the rules.
Working with a skilled billing company provides great benefits through their help with appeals and rules. So the right partner offering medical reimbursement service can help the provider’s team to improve revenue and feel more secure about claim submissions.
How can Medical Reimbursement Services optimize reimbursement rates?
The primary goal of a physician or any healthcare practice should be to provide high-quality healthcare services to patients. Achieving quality care requires the establishment and maintenance of well-trained staff, certified and experienced physicians, and advanced medical equipment.
However, all of this relies on revenue growth, which can be achieved by maximizing reimbursements from insurance providers or from uninsured patients.
Healthcare providers often face challenges when they do not receive timely payments due to issues such as incorrect coding, incomplete information in claims, or late submissions. Partnering with a full-service medical billing company can help overcome these obstacles and ensure a smoother revenue cycle.
A medical billing company’s medical reimbursement services play a crucial role in maximizing reimbursements by leveraging expert knowledge and strategic processes designed to capture every eligible dollar. Here’s how:
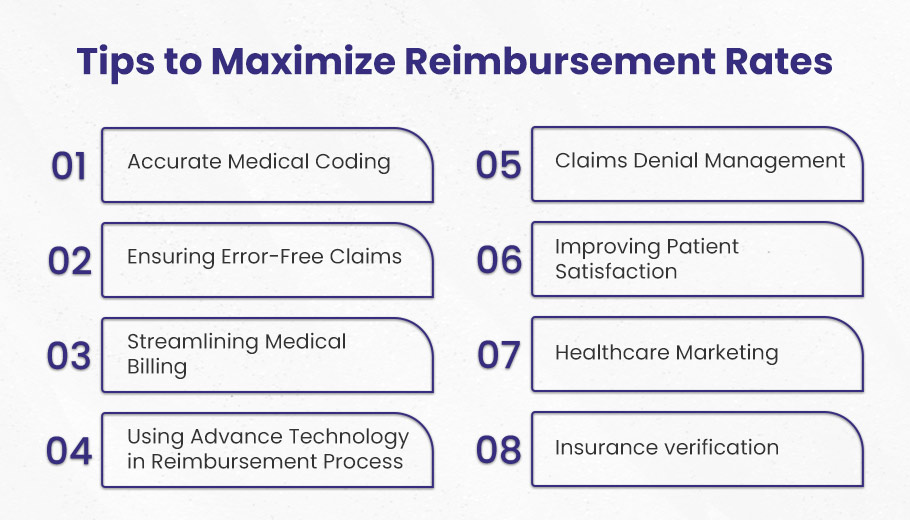
☑️ Implementing Accurate Medical Coding
You cannot deny the importance of accurate coding as it is a crucial part of the reimbursement process. Codes describe the medical services provided to patients. Entering right codes enable billers to prepare claims correctly which can ultimately result in reimbursement on time.
As a healthcare provider, outsourcing medical milling companies can assist you in overcoming healthcare reimbursement hurdles. They have expert coders and billers at their facilities who are regularly trained and educated in coding and billing for making them compliant with the latest guidelines and trends. Also, these professional coders stay updated with HIPAA, Medicare and Medicaid, and other regulatory authorities.
One of the best features of billing companies is that they regularly perform internal audits to identify any issues and solve them before a practice may become vulnerable to an external audit due to incorrect coding.
☑️ Ensuring Error-Free Claims Submission
Professional billers at medical billing companies avoid common mistakes such as entering incorrect patient information, wrong codes, missing details, duplicate billing, or billing for non-covered services, and filing claims after their estimated time. Avoiding these mistakes can help appropriate reimbursement which is helpful for practice and revenue growth.
☑️ Streamlining the Medical Billing Process
Medical reimbursement services help maximize reimbursement rates in several ways. One key way is by streamlining the medical billing process. This is critical for getting the highest reimbursement amounts in a timely manner.
Dedicated staff at outsourced billing companies overhaul the entire billing workflow. This starts from the initial submission of claims all the way through follow-ups and denial management. Streamlining this process boosts billing accuracy. It also accelerates the speed of reimbursements.
Specifically, streamlined billing includes steps like:
- Checking claims for errors and omissions before submission. This avoids rejections that lead to payment delays.
- Utilizing billing software to auto-populate claims with patient and procedural codes. This prevents manual data entry errors.
- Establishing workflows to submit claims electronically. This fast-tracks the reimbursement timeline versus paper claims.
- Setting up protocols for claim follow up at set intervals. This ensures quick resolution of any pending claims.
- Developing denial management procedures to swiftly resubmit denied claims. This maximizes the chance of reimbursement.
Optimized billing workflows are indispensable for maximizing reimbursement rates. Outsourced services dedicate staff and technology to remove all friction from billing. This pays big dividends in the form of faster and higher reimbursements.
☑️ Leveraging Advanced Technology
Today, medical practices must use technology to improve how they manage money and increase payment rates. Billing software and custom platforms help practices make the reimbursement process easier, from sending claims to collecting payments. Modern technology helps get the most money back for medical expenses. Here’s how:
Automated Claim Processing – Outsourced billing services use advanced software to auto-check claims for mistakes and process them rapidly for submission. This helps prevent rejections and delays.
Tracking and Analytics – Technology offers live dashboards to see claim status, reasons for denial, trends in reimbursement, and more. This data helps identify problem areas.
Coding Help – Smart coding tools suggest the right codes and modifiers to make sure claims are submitted correctly the first time. This stops reimbursement leaks from coding issues.
Patient Billing – Online patient portals allow easy self-pay collection. Automated payment reminders and follow-ups help to lower unpaid claims. This increases total payment income.
Compliance Checks – Billing platforms can identify compliance problems when coding and submitting. This helps prevent expensive audit fines or refunds.
So you see that using the latest billing technology is very important for practices today. It helps make the revenue cycle easier, reduces rejections and delays, and improves coding, compliance, and payment collection. This leads to more money being paid back and increased income. This is the reason why outsourcing billing to vendors using advanced platforms is an efficient way for practices to optimize their reimbursement performance.
☑️ Managing Claims Denials Effectively
Claims denial is one of the major reasons for revenue loss in healthcare practices. Timely claims denial management is crucial for sustaining and improving any medical practice. Outsourced medical billing companies can help providers minimize claim denials and maximize reimbursement rates through effective denial management strategies.
Here’s how it works:
◉ Careful Planning: Medical billers analyze past claims data to identify common reasons for denials. They then devise customized plans to prevent and tackle denials.
◉ Identifying Denial Reasons: Billers investigate denied claims to pinpoint the exact reasons, like missing information, improper coding, untimely filing etc. Knowing the reasons is key to appealing correctly.
◉ Gathering Information: Medical billers obtain any missing documentation or information required to support the denied claims. This includes clinical notes, re-coded claims, patient details etc.
◉ Filing Appeals: Billers draft appeal letters addressing the specific denial reasons and include all relevant facts and documentation. Well-written appeals have higher chances of overturning denials.
◉ Follow-up: Persistent follow-up is done until final resolution of the appealed claims.
☑️ Enhancing Patient Satisfaction
Improving patient satisfaction is key to increasing reimbursement rates for healthcare providers. This is because Medicare and many private insurers now tie reimbursement to patient satisfaction scores. Here’s a brief overview of how it works and why it’s so important:
What does it include?
▸ Communication – Making sure patients feel heard and understood at every interaction. This includes doctors, nurses, front desk staff, etc.
▸ Responsiveness – Answering questions, addressing concerns, and meeting needs in a timely manner. Patients should not feel ignored.
▸ Quality care – Providing competent, professional medical care from start to finish. This ensures patients are confident in the treatment they receive.
Why does it matter?
Higher patient satisfaction means higher reimbursement rates. Medicare payments are directly tied to Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, which are based on patient surveys. Many private insurers now do the same.
This means improving patient satisfaction across all touch points can have a big impact on the bottom line for healthcare organizations. Tracking satisfaction and continuously improving is key to maximizing reimbursement.
Medical reimbursement services help ensure that patients get correct and timely bills, improving their overall experience. They also help settle any payment problems or disagreements, which makes things easier for patients who are frustrated or confused.
☑️ Supporting Healthcare Marketing Efforts
Marketing is one of the most effective ways to reach patients who need your healthcare services. By implementing a robust marketing strategy, you can increase patient footfall to your healthcare practice.
Outsourced medical billing companies utilize various traditional and digital marketing platforms, including banners, social media, and pay-per-click (PPC) advertising campaigns.
Digital marketing, in particular, boosts your online presence, making it easier for patients to find you, as many now turn to the internet to search for care services. As a result, you can maximize reimbursements by treating more patients who are attracted to your practice through these marketing efforts.
☑️ Conducting Thorough Insurance Verification
Providing treatment services to ineligible patients can lead to significant financial losses due to unpaid claims. With medical reimbursement services, experts at billing companies meticulously review all patient credentials before you provide care. This process ensures that you deliver services only to eligible patients, allowing you to receive timely reimbursements.
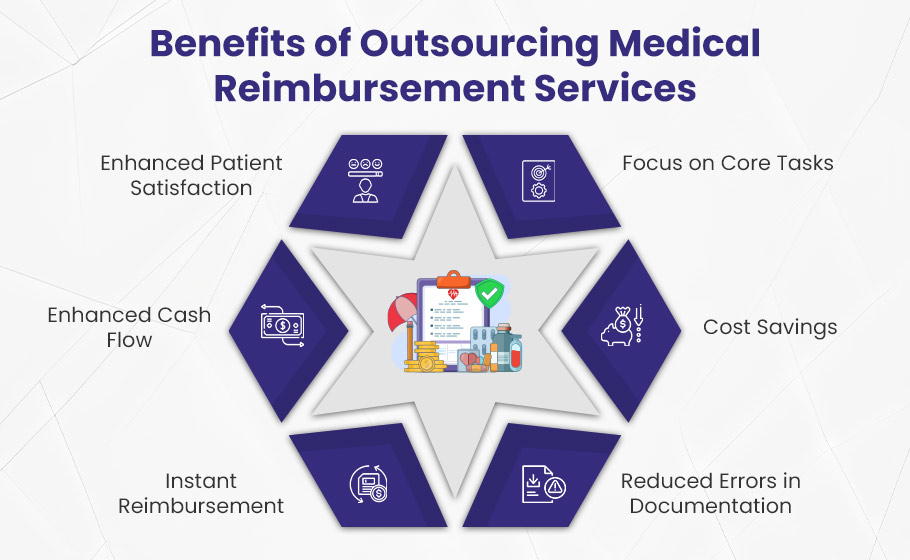
Benefits of Outsourcing Medical Reimbursement Services
We have discussed how partnering with a full-service medical billing company can help healthcare providers maximize their reimbursement rates. In this section, we will explore the key benefits of outsourcing medical reimbursement services to specialized billing companies.
Better Focus on Core Tasks
By outsourcing medical reimbursement services to experienced professionals, healthcare providers can concentrate on their core competencies, allowing more time for patient care. For instance, when physicians are overwhelmed with administrative tasks—like managing billing and claims—they may struggle to deliver quality care. By delegating these responsibilities to billing companies, providers can enhance patient satisfaction and improve the overall patient experience.
Cost Savings
One of the major benefits of outsourcing medical billing is cost savings. Managing an in-house billing team can incur excessive expenses, including salaries, benefits, training, and utilities. For example, a healthcare practice with a five-person billing team may face significant costs related to employee benefits and ongoing training. By hiring outsourced reimbursement services, providers can reduce these costs, optimize their revenue cycle management, and ultimately enhance the quality of care.
Reduced Errors in Documentation
Healthcare providers often face challenges in securing reimbursements when insurance companies deny or delay claims due to documentation errors. Professional billing companies employ certified experts who specialize in billing accuracy. For instance, a billing expert might identify and correct coding errors before submission, drastically reducing the chances of claim denials. Their extensive knowledge of complex medical terms and codes ensures a smoother revenue cycle with fewer mistakes.
Better Cash Flow
Outsourcing billing services can significantly improve cash flow for healthcare practices. By ensuring timely, error-free claims submissions and reducing the number of denied claims, billing companies help providers achieve steady financial growth. For example, a practice that previously experienced delays in payments might see improvements in cash flow within months of outsourcing, allowing them to invest in better equipment or staff.
Enhanced Patient Satisfaction
Patient satisfaction is crucial for the growth of healthcare practices. Professional billing companies improve billing accuracy, which contributes to better patient experiences. By streamlining administrative tasks and expediting claims processing, these companies ensure quicker reimbursements and reduce delays in providing patients with accurate treatment and financial records. For instance, if a patient receives clear and prompt billing information, they are more likely to feel confident in their healthcare provider.
Instant Reimbursement
Outsourcing to dedicated medical billing teams accelerates the reimbursement process. These teams consist of highly qualified professionals with extensive experience in addressing reimbursement issues for healthcare providers. For example, outsourced experts often complete claim submissions and follow-ups in a fraction of the time it would take an in-house team, reducing the overall wait for reimbursements. Typically, outsourced services can achieve reimbursements three times faster by effectively managing every stage of the claim process without errors.
Conclusion
Understanding medical reimbursement services is important for healthcare providers who want to increase their income and get paid on time for their services. The reimbursement system has different models like fee-for-service, capitation, and bundled payments. It is important to understand coding, rules, and financial reporting well.
| Criteria | Managing In-House | Outsourcing to Medical Billing Company |
| Cost Efficiency | ❌ Higher costs due to salaries, benefits, and training. | ✔️ Reduced overhead costs; pay only for services rendered. |
| Focus on Core Competencies | ❌ Time-consuming administrative tasks distract from patient care. | ✔️ Allows healthcare providers to focus on patient care and clinical responsibilities. |
| Expertise and Accuracy | ❌ Limited expertise may lead to frequent errors in billing and coding. | ✔️ Access to specialized billing experts who minimize errors and ensure accurate submissions. |
| Claim Denial Rates | ❌ Higher claim denial rates due to documentation errors. | ✔️ Lower denial rates as professionals understand regulations and coding intricacies. |
| Cash Flow | ❌ Slower cash flow due to potential delays in claims processing. | ✔️ Faster reimbursement cycles, improving overall cash flow. |
| Compliance and Regulatory Knowledge | ❌ Providers may lack up-to-date knowledge of regulations. | ✔️ Dedicated teams stay current with regulatory changes, ensuring compliance. |
| Scalability | ❌ Scaling an in-house team can be challenging and costly. | ✔️ Easily scalable services that adapt to the needs of the practice. |
| Technology and Tools | ❌ Investment in billing software and technology is necessary. | ✔️ Access to advanced billing software without the extra cost. |
| Patient Satisfaction | ❌ Administrative burdens can lead to longer wait times for patients. | ✔️ Improved billing accuracy and quicker resolutions enhance patient satisfaction. |
| Instant Reimbursement | ❌ Reimbursements may take longer due to inefficiencies. | ✔️ Streamlined processes often result in faster reimbursements. |
By using specialized medical billing companies, providers can make their claims processes easier, reduce the chances of denials, and improve their financial results. Using expert medical reimbursement services helps reduce administrative work. This allows healthcare practices to concentrate on providing good patient care. It also supports financial stability and better health results for the communities they help.