Credentialing takes time! But how long?
How long does it take to get credentialed with insurance companies and why?
The average time it takes for providers to get credentialed is between 90 to 120 days (and up to 180 days in some cases). Some insurance companies process applications faster, while others may take longer, especially for certain specialties.
So, the time frame varies significantly, depending on tons of factors. We’ll talk about them in detail as you scroll through.
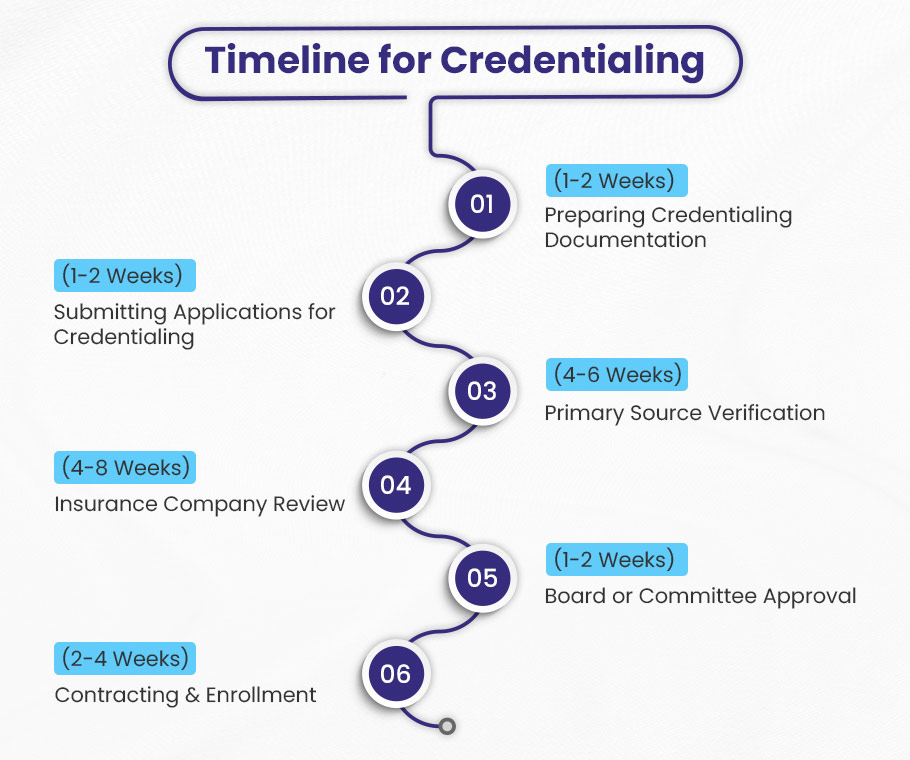
The Timeline for Provider Credentialing Process
The credentialing process for healthcare providers with insurance companies involves several key steps, each taking a specific amount of time.
Here’s a detailed timeline breakdown of the credentialing process.
| Step | Timeframe | Key Activities |
| 1. Preparing Documentation | 1-2 Weeks | Collecting necessary documents and ensuring accuracy. |
| 2. Submitting Applications | 1-2 Weeks | Filling out application forms, proofreading, and submitting them to insurance companies. |
| 3. Primary Source Verification | 4-6 Weeks | Verification of credentials with educational institutions, licensing boards, and previous employers. |
| 4. Insurance Company Review | 4-8 Weeks | Detailed review of the application for compliance and background verification. |
| 5. Board or Committee Approval | 1-2 Weeks | Presentation of the application to the credentialing committee for evaluation and decision-making. |
| 6. Contracting and Enrollment | 2-4 Weeks | Reviewing and signing the contract to finalize enrollment in the insurance network. |
| Total Duration | 12-24 Weeks | Overall time can vary based on application completeness, verification responsiveness, and internal processes. |
You Gotta Get Cred ASAP! 💰
You’re a boss, so start getting paid like one. BellMedEx’s credentialing experts will get you legally approved to start raking in those insurance dollars.
1. Preparing Documentation (1-2 Weeks)
The initial step involves collecting all necessary documents that may take 1-2 weeks. A credentialing specialist can review these documents thoroughly who also conducts primary source verification to ensure accuracy.
Providers should prepare a checklist to streamline this phase.
Application: General information including personal details, contact information, and professional background.
Education: Documentation of education such as diplomas, specialty certificates, and additional qualifications.
Licenses and Certifications: Copies of current and valid medical licenses, board certifications, and registrations.
Work History: Detailed account of previous positions, dates of employment, and responsibilities.
Malpractice Insurance: Proof of malpractice or liability insurance coverage.
References: Professional references from colleagues, supervisors, or mentors.
DEA Registration: Drug Enforcement Administration registration details for prescribing controlled substances.
Personal Identification: Valid identification documents like a driver’s license, passport, or social security number.
Background Check: Verification of criminal records and/or disciplinary actions.
Credential Evaluation: Assessment against the organization’s specific criteria.
Preparing and gathering necessary documentation helps streamline the credentialing process and avoid delays.
2. Submitting Applications (1-2 Weeks)
After gathering documents, providers fill out application forms for getting credentialed with insurance companies. This step includes gathering personal details, filling in required information, reviewing for accuracy, and submitting the applications. Generally, it takes 1-2 weeks, but using robust credentialing software speeds up the process.
- Get personal, professional, and supporting documents (1-2 Days).
- Fill out the application forms and start leveraging software (3-5 Days).
- Proofread and review the entire application once again (1-2 Days).
- Submit the application with methods specified by insurance companies (1-2 Days).
- Track submissions, respond to requests, and follow up with the insurance companies (ongoing).
Using the right tools and strategies helps you manage, complete and submit applications effectively within the 1-2 week timeframe.
3. Primary Source Verification (4-6 Weeks)
During this crucial phase, insurance companies verify credentials directly with educational institutions, licensing boards, and previous employers. This credentialing step ensures the accuracy and authenticity of the provider’s qualifications.
The time frame can vary depending on the responsiveness of the institutions and agencies involved. But generally, it takes around 4-6 weeks. You can do nothing about it, just make sure you give accurate information and truthful documentation.
4. Insurance Company Review (4-8 Weeks)
Once verification is complete, the insurance company reviews the application in detail. This includes checking compliance with their internal standards. The time frame is usually 4-8 weeks but can vary based on the thoroughness of their review process.
The insurance company reviews the application, assessing the provider’s qualifications, experience, and background. The process may include:
- Application Assessment
- Compliance Check
- Background Verification
- Internal Review Timelines
Delays can occur if the insurance company needs further clarification or if there are issues with the documentation provided. It can also take long if the insurance company’s internal review committees meet less frequently.
5. Board or Committee Approval (1-2 Weeks)
The application is then presented to a credentialing committee or board, which meets monthly or bi-monthly. It evaluates all findings and makes a decision on the provider’s credentialing status.
The timing of the next available meeting can influence how quickly the application is reviewed. But usually, this step in the provider credentialing process takes 1 to 2 weeks approximately. You cannot do anything to expedite the process.
The credentialing committee typically includes healthcare professionals and administrative staff, and it reviews the application in detail. They assess qualifications, experience, and findings from the background checks and compliance reviews.
After the committee review, the members raise concerns and talk about the provider’s suitability for inclusion in the network. And then, they vote on whether to approve, deny the application, or request some more information.
If approved, you’re done with the initial credentialing process and get in-network with the insurance. But if the additional information is required, the process gets extended until the next committee meeting.
6. Contracting and Enrollment (2-4 Weeks)
After approval, you as a healthcare provider will receive and review a contract outlining participation terms. You can negotiate before signing. Once signed, you are officially enrolled in the insurance network.
The insurance company updates their systems to include you as a new provider in their network. This ensures that patients and other stakeholders can see that the provider is now part of the network. The provider receives a notification confirming their enrollment.
This step in credentialing typically takes 2-4 weeks to complete, depending on the efficiency of both the provider and the insurance company.
In total, the entire credentialing process can take between 12 to 24 weeks (approximately 3 to 6 months), depending on these factors:
- The completeness of the application.
- The responsiveness of third-party verification sources.
- And internal processing times of the insurance company.
Level Up Your Credentialing Game! 🎯
Waiting to get credentialed is a total buzz-kill. Don’t let the insurance companies leave you hanging – get that credentialing process started NOW before it’s too late. We’ll show you how to speed things up so you can get paid, pronto!
But why does the credentialing take ages? Let us answer that!

Why Does Provider Credentialing Take So Long?
As a healthcare provider, you’ve jumped through all the hoops – submitting your application, paying fees, providing documents – to get credentialed. But instead of the few weeks you expected, it’s been months, and your insurance credentialing status is still stuck in limbo. What gives?
You’re not the problem. The snail’s pace is by design on the insurers’ part.
Insurance companies follow a lengthy, rigorous credentialing process to vet every provider before allowing them to join their network. This involves verifying your qualifications, work history, malpractice coverage, and other aspects that affect your ability to deliver safe, quality care. They must comb through primary source verifications, license checks, and other certifications.
So while frustrating for providers, the long credentialing timeframe stems from the insurer’s due diligence. For you, it means playing the waiting game.
Here’s an overview of what contributes to these delays.
➡️ Extensive Verification
Credentialing requires thorough verification of a provider’s education, training, licenses, certifications, work history, and malpractice records. This process involves contacting multiple institutions, which can take time.
➡️ Primary Source Verification
Each piece of information must be confirmed directly with original sources, such as medical schools, licensing boards, and other institutions. This step ensures accuracy but lengthens the timeline of provider credentialing.
➡️ Background Checks
Comprehensive background checks, including criminal history and malpractice verification, are crucial for patient safety. These checks can take considerable time to complete, making sense of prolonged credentialing timeframe.
➡️ Committee Reviews
Credentialing committees need to review and approve applications. Delays can occur if there are scheduling conflicts or backlogs of applications in the review process.
➡️ Incomplete Applications
Missing or incorrect information in a provider’s application can cause significant delays. Requests for additional documentation or corrections can add weeks or even months.
➡️ Lack of Standardization
Different healthcare facilities may have varying requirements and processes for credentialing. There’s no standardization and this creates redundancy and inefficiencies, prolonging the process.
➡️ High Volume of Providers
When many providers are seeking credentialing at the same time, backlogs can develop, slowing down the overall process.
➡️ Response Times from Institutions
Delays can occur if educational institutions or previous employers take too long to respond to verification requests. A slow response can add weeks to the provider credentialing timeline.
➡️ Discrepancies in Documentation
Additional follow-ups are required if there are discrepancies in the information provided. Investigating these issues can significantly extend the credentialing process.
➡️ Scheduling Conflicts
If the credentialing board has a busy schedule, it may take longer to get applications reviewed and approved.
➡️ Internal Processing Delays
The insurance company or healthcare facility may have internal processing delays due to staffing, policy changes, or procedural bottlenecks.
Tips to Speed Up Insurance Credentialing Process
To expedite the credentialing process, providers must start the process earlier, use robust software, establish a clear workflow, set reminders for follow-up, and hire a good healthcare credentialing company.
✅ Streamline Documentation
To speed up the insurance credentialing process, healthcare providers can follow these steps to improve how they handle and submit their application documents:
➜ Organize Your Documents: Create a list of all the documents you need, like insurance information, licenses, and certificates. Put them in a special folder so you can get to them easily.
➜ Use Standard forms: Submit documents in widely accepted formats (like PDF). This reduces confusion and makes it easier for insurance companies to review your materials.
➜ Double-Check Everything: Make sure all of your documents are complete and accurate before sending them in. Delays can happen when information is missing or wrong.
➜ Digital Submission: Whenever possible, submit applications and documents electronically. This speeds up the process and reduces the risk of lost paperwork.
➜ Follow Up: Once you’ve sent your documents to the insurance company, call them again to make sure they got them and to find out what’s going on with your application.
✅ Conduct Pre-Credentialing Reviews
Conducting pre-credentialing reviews is an effective way to speed up the credentialing process. By taking proactive steps, you can ensure that everything is in order before submitting applications.
➜ Use Pre-Screening Checklists:
- Develop checklists that list all the necessary documents and information needed for credentialing.
- Check these lists to identify any missing items or potential issues before you submit the application.
➜ Hold Mock Credentialing Sessions:
- Conduct practice sessions that simulate the credentialing process.
- Use these sessions to spot any bottlenecks or problems that might slow down the process.
✅ Engage a Credentialing Service
As a healthcare worker, you can get outside help to speed things up if you need to.
Using third-party companies that offer credentialing services is one strategy. These businesses already have systems in place and connections with payers that make the credentialing process go faster. As part of their routine work, they fill out forms, check papers, and follow up with insurance companies. Because of this, you will be able to focus more on each patient.
Working together with a Managed Service Organization (MSO) is another choice. MSOs offer full credentialing support as one of their many services. Some of the things they do to help you get accepted are talking to payers, filing claims, negotiating contracts, and managing the medical revenue cycle. This all-around service makes sure that your credentials are always up-to-date and that you get paid quickly for your claims.
⏳ ❝ Tick-tock, tick-tock… ❞
It doesn’t have to be this way!
With BellMedEx, the credentialing process becomes hassle-free, enabling you to see more patients and improve your reimbursement turnaround!
✅ Strengthen Relationships with Payers
Healthcare providers should focus on building better connections with payers to speed up the insurance credentialing process. This means keeping in regular contact with payer officials and quickly informing them about any changes that could affect credentialing.
Here are some key areas for providers to focus on:
- ➜ Talk Directly to Payer Staff: Reach out to the payer credentialing team. This can help clarify any confusing requirements and ensure you understand what’s needed. Having a specific contact person can also make it easier to check on the status of your applications and resolve any issues that might delay acceptance.
- ➜ Keep Payers Updated: It’s important to inform payers about any changes to your details. This includes updates to credentials, locations, affiliations, licenses, and more. By giving timely notice, payers can quickly update their records, which helps prevent administrative hiccups that could slow down the process.
By sharing clear information and delivering frequent updates, providers can groove their way to solid relationships with payers. This not only jazzes up the credentialing process but also lets providers get the green light faster, so they can jump right into caring for patients with insurance coverage.
credentialing can take
❝ fooorrrreeeevvveerrrr…❞
We are here to help! 🤗
You’ve submitted your credentialing paperwork, but now you have to wait for what feels like an eternity with no real timeline? Ugh, we feel your pain! BellMedEx will put you on the fast track to getting fully credentialed.