Healthcare provider credentialing is complex and thus takes 3 to 6 months. That is why more healthcare facilities are opting for DELEGATED CREDENTIALING.
It increases enrollment turnaround times, decreases paperwork, and expedites timely reimbursement. The insurance company also takes less time to decide whether to take a provider on its panel or not.
This comprehensive guide will help you understand everything you need to know about delegated enrollment and credentialing.
What is Delegated Credentialing?
Delegated credentialing is an arrangement in which a healthcare entity gives its credentialing authority to another healthcare entity. For example, a preferred provider organization may legally ask a hospital to credential its providers.
The delegated healthcare entity becomes responsible for taking credentialing decisions on the delegating healthcare entity’s behalf. They can verify provider’s qualifications, state licensure, DEA registration, work history, and more.
A delegated healthcare entity is responsible for reviewing and analyzing provider’s qualifications and making credentialing decisions on behalf of delegating entities.
The delegated entity may require this data:
- Professional Liability Claims Settlement History
- CDS (Controlled Dangerous Substance) Certification
- Education Malpractice History
- DEA Registration
- Sanctions & Exclusions
- Disclosure Questions
- Board Certification
- State Licensure
- Work History
- Hospital
- Attestation
But remember that a delegating entity is ultimately responsible for compliance with regulatory bodies, federal, and state laws.
Who Can Delegate Credentialing and Be Delegated?
There are two major healthcare entities involved in delegated credentialing:
- Delegated entity
- Delegating entity
These healthcare organizations can be delegated:
- Provider Groups (single or multi-specialty or multi-location)
- Independent Physician Associations (IPA’s)
- Hospitals & Hospital Systems
- Specialty Provider Networks (Dental, Vision)
And these healthcare organizations can delegate:
- Provider Networks
- Independent Physician Associations (IPA’s)
- Preferred Provider Organizations (PPO)
- Health Plans (Cigna, Aetna, etc)
- Accountable Care Organizations (ACO’s)
- Specialty Provider Networks (Dental, Vision)
Fun Fact: Some entities like IPAs and SPNs can delegate and be delegated as well.
Not sure whether your healthcare organization can delegate or be delegated? Schedule a free consultation session now to learn everything you need before getting started with delegated credentialing.
Some Examples of Delegated Credentialing
Delegated credentialing is an arrangement where one healthcare organization lets another organization handle the credentialing process for them. It’s a way to streamline things by having a larger entity take care of the administrative work for smaller groups. Let’s look at a few examples to understand it better:
Example #1
Dr. Smith works at Community Hospital but also sees patients at the local clinic run by Metro Health Network. Instead of Dr. Smith having to go through credentialing twice, Metro Health allows Community Hospital to credential him on their behalf. This saves time and duplication of efforts.
Example #2
As another example, many health insurance plans don’t directly employ physicians. Instead, they contract with independent doctor groups and healthcare organizations to provide care for their members.
The insurance plan will delegate the credentialing of those outside doctors and groups to a third-party credentialing agency. That agency becomes responsible for ensuring all the doctors meet the insurance plan’s requirements before they can officially join the plan’s network.
This helps the insurance plan quickly build a network of high-quality doctors without investing in their own credentialing department.
What is a Delegated Provider in Credentialing?
A delegated provider in credentialing refers to the provider that was given the responsibility of credentialing another provider or organization. That is not usually the individual provider but a full-fledged healthcare organization.
What is an Authorized Agent?
Authorized agent is any entity elected by eligible healthcare entities to process delegated credentialing and query the NPDB (National Practitioner Data Bank) on their behalf. Remember the authorized agents may act for more than one entity.
What is a Delegated Entity in Healthcare?
Delegated entity in healthcare is the entity to which the administrative responsibilities were delegated by another healthcare entity (called the delegating entity). However, the delegating entity oversees the entire process to ensure accuracy and compliance.
A delegated credentialing entity is any party that enters into a delegated credentialing agreement with a delegating entity. It’s the entity that has been given the authority to credential the healthcare providers of a (delegating) credentialing entity.
What is a Delegated Credentialing Agreement?
A delegated credentialing agreement is a written document that outlines all the credentialing responsibilities to delegated and delegating entities. The agreement is important because some functions in credentialing remain in-house. But mostly, the entire credentialing process is delegated to an entity.
The agreement for delegated credentialing also details down the managed care standards, termination rights, required reporting, and more. For example, the required reporting section of the agreement shares things that need to be reported, including complaint monitoring, semiannual credentialing activity, and more.
Delegated vs Non Delegated Provider in Healthcare
The difference between delegated and non delegated providers in healthcare credentialing is the existence of delegated credentialing entities. Non-delegated providers are the ones whose credentialing is done by their associated healthcare facility. The process is called credentialing.
In non-delegated credentialing, the healthcare facility collects credentialing information from its associated providers for their credentialing. In delegated credentialing, the outside entity does this job in accordance with the written agreement.
Delegated Credentialing vs Credentialing by Proxy
Delegated credentialing transfers the credentialing authority from one entity to another, while credentialing by proxy (CBP) refers to the credentialing of telehealth or virtual healthcare practitioners.
CBP allows the prime source verification, meaning hospitals using virtual healthcare services can accept the credentialing work of the remote hospital. They don’t need to implement the full credentialing for providers who never visited or sit in the hospital.
Regulatory Bodies Involved in Delegated Credentialing
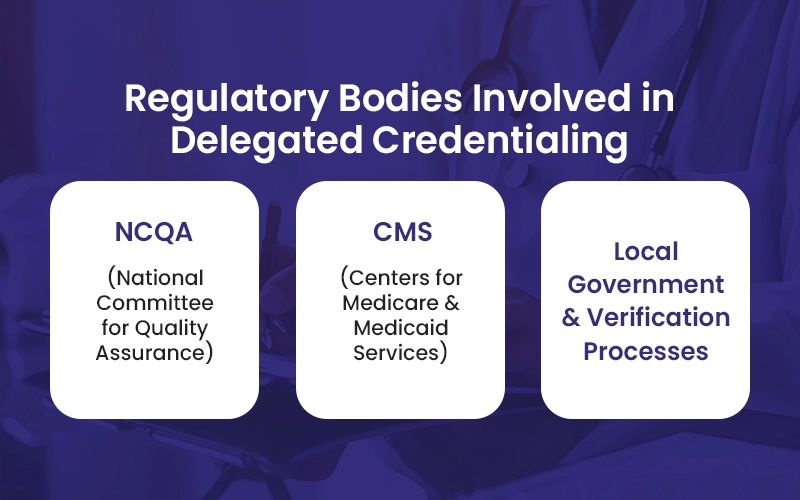
There are three major regulatory bodies and stakeholders that ensure quality, compliance, and patient safety in delegated credentialing.
1. NCQA (National Committee for Quality Assurance)
NCQA sets standards for healthcare quality and performance improvement. Their guidelines are considered crucial in ensuring that credentialing processes meet high standards of reliability and accuracy. Healthcare organizations align their practices with NCQA standards to increase credibility and quality assurance.
2. CMS (Centers for Medicare & Medicaid Services)
CMS oversees federal healthcare programs including Medicare, Medicaid, CHIP, and ACA-related initiatives. It also imposes regulatory requirements for healthcare entities involved in delegated credentialing, complying with federal laws, safeguarding patients, and ensuring billing integrity.
3. Local Government and Verification Processes
Healthcare entities and authorized agents may need to follow some rules set by local governments. For example, you need to verify credentials directly from primary sources such as medical schools, licensing boards, and previous employers. Meeting deadlines and following such guidelines are important in obtaining and maintaining delegated credentialing status at the local level.
Delegated Credentialing Requirements for Time
The NCQA and other regulatory agencies have many requirements and standards. And the most important ones are being strict on time frames for the primary source verifications (PSV) as listed below.
| Type | Time |
| Current License | 180 days |
| Federal DEA and/or CDS Certificate | No set PSV time limit. Must be obtained before the committee decision date. |
| Board Certification | 180 days |
| Education and Training | No set PSV time limit. Must be obtained before the committee decision date. |
| Malpractice History | 180 days |
| Work History | 365 days |
This is just the PSV time requirement, look up the delegated credentialing agreement for a comprehensive list of requirements.
Delegated Credentialing Process (How Does Delegated Credentialing Work)
Your healthcare facility must abide by different requirements, especially set by NCQA, to participate in a delegated credentialing arrangement.
Delegating entities can also set their own standards for delegated credentialing.
Setting and following the process is important also because the regulatory bodies require certain elements for delegated credentialing, such as pre-delegated assessment, oversight audits, and more.
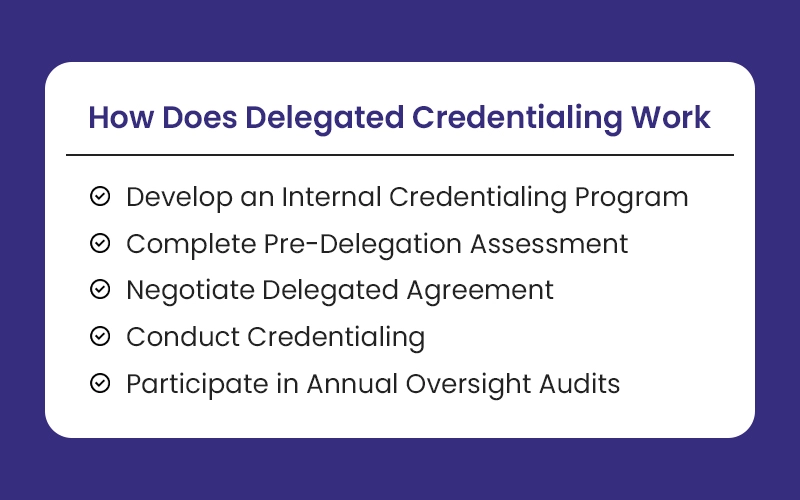
Here’s how to implement delegated credentialing:
1. Develop an Internal Credentialing Program
Make policies and procedures compliant with state, federal, and payer regulations. Establish a robust quality oversight program involving medical staff services, quality department, peer review committees, and other stakeholders. Allocate necessary resources including personnel, operational infrastructure, and credentialing software.
2. Complete Pre-Delegation Assessment
Conduct an initial audit to evaluate policies and procedures against NCQA, URAC, or CMS managed care standards. Review a sample of initial and re-credentialing files to ensure compliance with credentialing criteria. Assess staffing levels and performance capabilities to ensure all processes align with regulatory requirements.
3. Negotiate Delegated Agreement
Define and document the responsibilities of both parties (health plan or delegating entity and delegated entity) about credentialing activities. Agree on the frequency, content, and format of credentialing activity reports to be submitted to the health plan.
Clearly decide on how you will analyze performance and resolve non-compliance issues. Determine reimbursement rates and fee structures applicable under the delegated credentialing agreement.
4. Conduct Credentialing
Utilize a robust credentialing software to verify qualifications, licenses, certifications, and other credentials of healthcare providers. Maintain accurate and up-to-date provider rosters detailing status changes, new enrollments, and terminations. Submit provider rosters to health plans in the required format and within specified timelines.
5. Participate in Annual Oversight Audits
Prepare for annual oversight audits conducted by NCQA, CMS, or health plans to evaluate compliance with credentialing standards. Review policies, procedures, and credentialing files to ensure adherence to regulatory and accreditation requirements. And in case of any discrepancies, implement corrective action plans to maintain compliance and contractual obligations.
Pros and Cons of Delegated Credentialing
Delegated credentialing offers many benefits but also requires careful management of responsibilities, compliance, and oversight to ensure smooth operation.
Benefits of Delegated Credentialing
- Saves time and resources for health plans overwhelmed with new enrollments.
- Lowers costs compared to hiring internal credentialing staff.
- Reduces turnaround time, allowing quicker enrollment of providers.
- Leads to quicker reimbursements for delegating entities.
- Enables new providers to start quickly, improving patient care.
Downsides of Delegated Credentialing
- Health plans (delegating entities) may lose control over credentialing quality.
- Changes in payer requirements can cause confusion if not managed carefully.
- Delegating entities bear responsibility for credentialing decisions.
- Many health plans mandate NCQA accreditation for delegates.
- Routine NCQA audits add to administrative burdens.
Streamline Delegated Credentialing With BellMedEx
BellMedEx offers comprehensive delegated credentialing services and can act as an authorized agent to streamline all things credentialing and enrollment. We optimize the delegated credentialing process for healthcare organizations to ensure efficiency and accuracy, compliance, and administrative relief.
Get free consultation on how we can help you improve your revenue cycle and increase patient satisfaction with our leading delegated credentialing solutions.




