Healthcare providers must tackle confusing codes in medical billing, each of which denotes certain services, processes, or problems with healthcare reimbursement. The CO-45 code is one of many that has seen its fair share of usage and abuse. It is a particularly noteworthy code. This coding, which frequently labels a claim as exploratory, investigative, or inaccurate, can be contentious. This article discusses the CO-45 Codes in medical billing, the implications, and measures to prevent errors.
CO-45 in Medical Billing
Medical billing is a complex process that involves multiple codes, regulations, and policies. One of the codes used in medical billing is CO-45. This code is used when a medical procedure or service is considered experimental or investigational and is denied by insurance providers.
Role of CO-45 Code
Medical billing is a complex process that involves multiple codes, regulations, and policies. One of the codes used in medical billing is CO-45. This code is used when a medical procedure or service is considered experimental or investigational and is denied by insurance providers.
CO-45 is a specific HCPCS code used in medical billing to indicate a corrected Medicare replacement claim. When a Medicare beneficiary’s initial claim is denied due to incorrect submission, the provider can submit a corrected claim with the CO-45 code to indicate a replacement claim being submitted to correct errors or omissions in the original claim. Using this code helps ensure that the corrected claim is processed correctly and that any necessary adjustments to the payment are made. However, it is essential to note that the CO-45 code should only be used for replacement claims submitted to correct errors or omissions in the original claim and not for initial claims or claims requiring additional information or documentation to be submitted. Medical billing and coding professionals need to understand the appropriate use of the CO-45 code to ensure accurate and efficient claim processing.
The CO-45 code is used in medical billing and coding when a Medicare beneficiary’s initial claim is denied due to incorrect submission. In such cases, the provider can submit a corrected claim with the CO-45 code to indicate a replacement claim being submitted to correct errors or omissions in the original claim.
For example, the initial claim may be denied if a provider submits a claim with incorrect patient information or diagnosis codes. In this case, the provider can offer a replacement claim with the CO-45 code to correct the errors and ensure the claim is processed correctly.
It is important to note that the CO-45 code should only be used for replacement claims submitted to correct errors or omissions in the original claim. It should not be used for initial claims or claims requiring additional information or documentation to be submitted. Understanding the appropriate use of the CO-45 code is essential to ensure accurate and efficient claim processing.
After learning about the CO-45 code in medical billing, it’s essential to know why the CO-45 code is used.
Implications of CO-45
By using the CO-45 code, it is possible to guarantee that the corrected claim will be handled correctly and that any necessary payment modifications will be made. The CO-45 code should only be applied to replacement claims submitted to remedy inaccuracies or omissions in the original claim. It is crucial to highlight.
Correcting Errors
When there are mistakes in the initial claim, the CO-45 code is applied. Errors like erroneous patient information, diagnoses, procedures, or billing codes can be fixed with it. Providers can correct the mistakes and resubmit the claim using this code to ensure it is appropriately processed.
Submitting a Replacement Claim
When submitting a replacement claim with the CO-45 code, providers must include all appropriate HCPCS codes to describe the services provided. Including any necessary documentation to support the claim and ensure it is processed correctly is also essential.
Avoiding Misuse of CO-45 Code
It is important to note that the CO-45 code should not be used for initial claims or claims requiring additional information or documentation to be submitted. Misuse of this code can result in claim denials or delays in payment.
Impact of CO-45 Code on Medical Billing
CO-45 code can significantly impact medical billing for healthcare providers. If a claim is denied due to this code, the healthcare provider will not receive reimbursement for the service provided. This can result in significant financial losses for the healthcare provider. It is essential to accurately document and code all services provided to minimize the risk of denied claims due to the CO-45 code.
Identifying CO-45 Code Issues
The first step in resolving CO-45 code issues is identifying the problems that must be addressed. This may include issues related to the appropriate use of the code, incorrect submission of claims, claim denials, or payment delays.
Working with Medicare
Once the issues have been identified, working with Medicare to resolve them is essential. This may include contacting the Medicare Administrative Contractor (MAC) or the Medicare Claims Processing Contractor (CPC) to obtain information or assistance resolving the issues.
Reviewing Claims
Providers should also review their claims to ensure that they are submitting claims correctly and using the CO-45 code appropriately. This may include reviewing claims for errors or omissions, ensuring that all appropriate HCPCS codes are included, and including any necessary documentation to support the claim.
Correcting Errors
If errors or omissions are identified, providers should correct the errors and resubmit the claim with the CO-45 code. Ensuring that the corrected claim is complete and accurate and that all necessary documentation is included to support the claim is essential.
How to Avoid CO-45 Code Errors
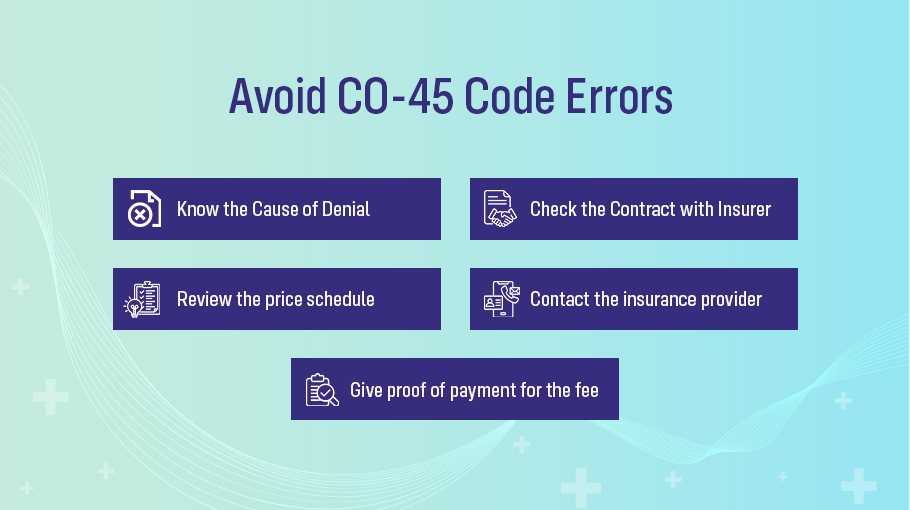
Healthcare providers should follow the measures below to prevent CO-45 denial and reduce errors:
- To determine the cause of the denial and the extent of the write-off, review the insurance company’s Explanation of Benefits (EOB) statement.
- Check your contract with the insurance provider to confirm that the invoiced amount is within the permitted amount.
- Review the price schedule for the specific treatment in the area to ensure the fee charged is reasonable and typical if the invoiced amount exceeds the allowable amount.
- Contact the insurance provider to discuss the denial and ask for a reconsideration of the claim if the fee is within the reasonable and typical range.
- Give proof of payment for the fee, such as a fee schedule, an invoice, or medical records.
Healthcare providers may challenge the insurance company’s decision or pursue a dispute resolution if the claim is still denied.
How To Appeal Co-45 Code?
When you receive a CO-45 refusal code, you can appeal if you think it is unfair or wrong. Check the claim status first to see if the payment was applied to the patient’s deductible or coinsurance. If not, you can send the insurance company an appeal request and relevant supporting materials.
A copy of the claim, the contract, an explanation of why you think the denial was incorrect, and any documentation that backs up your claim should all be included. Additionally, you must adhere to the insurance company’s appeal procedures and time constraints. You can submit the appeal to the insurance provider within 120 days. You can apply online via an official portal or email by providing the required documents.
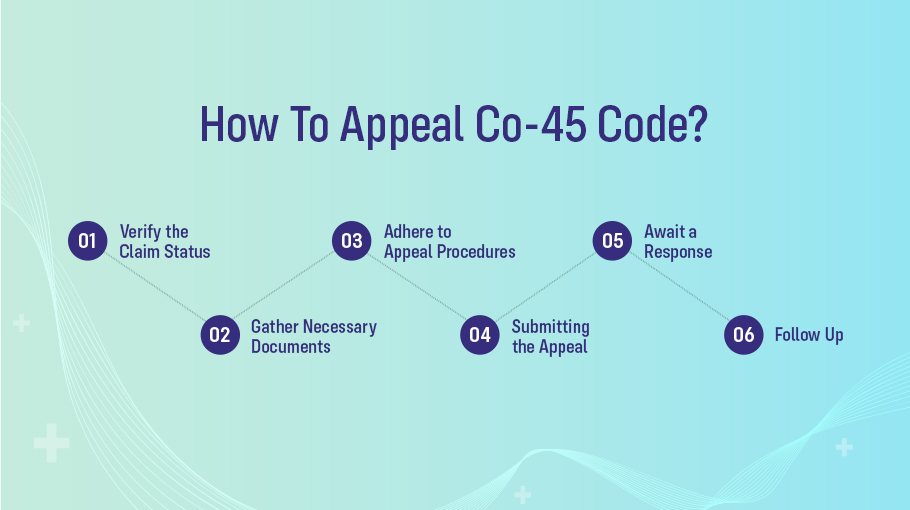
Receiving a CO-45 denial code on your medical claim isn’t the end of the road. You have the right to appeal if you believe the denial is unjust or incorrect. Here’s a step-by-step guide on how to navigate the appeal process:
Verify the Claim Status
Before proceeding, ensure the payment wasn’t applied toward the patient’s deductible or coinsurance. If it wasn’t, you can initiate the appeal process.
Gather Necessary Documents
Original Claim
Make sure to have a copy of the claim that received the CO-45 denial code.
Contractual Agreement
If the service was rendered based on a specific agreement with the insurance, have a copy at hand.
Reasoning for Appeal
Write a concise explanation detailing why you believe the denial was incorrect.
Supporting Documentation
This can include medical records, referral letters, lab results, or any other material that validates your claim.
Adhere to the Insurance’s Appeal Procedures
- Familiarize yourself with the insurance company’s appeal procedures. Every insurer has a specific process, so ensure you’re following the guidelines they’ve set.
- Be mindful of time. Typically, you have up to 120 days to submit your appeal. However, always check the insurer’s specific time frame to avoid complications.
Submitting the Appeal
Online
Some insurance companies have official portals to lodge your appeal. Make sure you have digital copies of all your supporting documents.
Via Email
If the insurer accepts email appeals, ensure you’ve attached all the necessary documents and send them to the designated email address.
[Note: Always keep a record of the appeal, whether it’s a screenshot, a confirmation email, or any other acknowledgment.]
Await a Response
Once submitted, the insurance provider will review your appeal. This can take anywhere from a few weeks to a few months, depending on the insurer’s process and the complexity of the request.
Follow Up
Don’t hesitate to follow up if you don’t hear back within the insurer’s specified timeframe. Ensure you have all the details of your original appeal when doing so.
Remember, the key is to be concise and provide all the necessary information to support your case. With the right approach and documentation, you stand a good chance of having the denial overturned.
Conclusion
Accuracy is a critical factor in the medical billing field. Amongst the various codes, CO-45 stands out due to its implications on reimbursement and the potential ramifications of its misuse. Understanding CO-45 is not just about decoding its definition but also about recognizing its broader impact on healthcare delivery, patient accessibility, and the financial dynamics of healthcare providers. By adhering to best practices, regularly updating knowledge, and ensuring rigorous documentation, healthcare establishments can safeguard against pitfalls associated with CO-45, ensuring that they continue to provide top-notch care without financial impediments.