Accurate and timely claim processing is crucial for smooth operations in healthcare. The UB-04 claim form, also known as the UB92 or CMS-1450 form, plays an important role in this process, serving as the standardized format for submitting medical billing claims to insurance companies by institutional healthcare providers.
Any healthcare provider filling out false or fraudulent information in the claim for payment is guilty of a crime and may be subject to heavy fines and confinement in prison. It also damages your healthcare facility’s reputation in the area, causing the revenue to drop as well.
That’s why it’s important to fully understand the UB-04 claim form. We’ll provide healthcare providers with the knowledge and instructions to use the UB-04 claim form and ensure proper reimbursement for services rendered.
About UB-04 Claim Form
The UB-04 form, previously called the CMS-1450 form, is the standard claim form used by an institutional healthcare provider to submit inpatient and outpatient medical claims for reimbursement from insurance companies when a provider qualifies for a waiver from the ASCA requirement for electronic submission of claims.
Key Points about UB-04 Claim Form:
- The National Uniform Billing Committee (NUBC) oversees the development and updates of the UB-04 form, ensuring its consistency and compliance.
- The purpose of the UB-04 claim form is to maintain the official record of all reimbursable care received by patients, allowing healthcare providers to bill Medicare, Medicaid, and other prayers for inpatient and outpatient services.
- The UB-04 form is widely adopted in healthcare. Over 98% of Medicare claims and more than 80% of all institutional claims use the UB-04 form.
- The UB-04 claim form is particularly used by institutional providers like hospitals, nursing homes, rural health clinics, and rehabilitation centers.
- The UB-04 form includes specific fields or boxes for providers to enter their NPI, facilitating accurate identification and streamlined communication with payers.
History
Back in the 1980s, the UB92 form was the go-to for hospital billing. But as time passed, it became outdated, and in 2007, the UB04 form stepped in to fix things. Developed by the NUBC and CMS, it offered more space for details, additional data fields, and a much easier-to-use format. Today, the UB04 is the standard for billing hospital services, making things smoother for both healthcare providers and insurance companies.
Importance and Usage
Treating patients is difficult work. Getting paid properly for treating those patients shouldn’t have to be. That’s the idea behind the UB-04 form.
It’s the standard billing document hospitals and clinics submit to insurance companies to receive reimbursement for inpatient and outpatient care they’ve already provided.
A well-crafted UB-04 tells the insurance companies in clear terms exactly which services and treatments were delivered to which patients, and the precise costs involved.
When healthcare providers take care to fully and accurately complete the UB-04, it streamlines the payment process and reduces the likelihood of denied or delayed claims.
The UB-04 aims to make medical billing more efficient so healthcare providers can focus on healthcare. After all, they got into medicine to treat patients, not to battle with insurance companies over payment. The UB-04 form helps them do a bit less of the latter.
Have a look at these points showing the importance of UB-04 in medical billing:

1). Streamlines communication between the provider and the insurance payer.
The UB-04 claim form provides a standardized format and medical codes (ICD-10 for diagnoses and CPT/HCPCS for procedures) for capturing and communicating billing information, ensuring clarity and efficiency.
For example, if a patient has a heart attack, the doctor will record the code for acute myocardial infarction, the proper name for a heart attack. They’ll also list codes for any procedures like CPR, medications, or time in intensive care. The insurance people see the codes and understand right off what happened and how the doctor handled it. Without the UB-04, the patient’s claim would be a mess of long descriptions and illegible handwriting. The UB-04 form makes it all as simple and orderly as possible.
2). Ensures the provider is accurately reimbursed for their services to the patient.
Accurately documenting services and charges in the UB-04 form helps providers receive the correct payment for their healthcare services.
For instance, a woman comes to see the doctor with a nasty cough that won’t go away. He listens to her lungs, checks her temperature, maybe does an X-ray. He’ll write out each step he took, and how much it set her back.
‘Examined patient, noted congested lungs and elevated temperature. Took chest X-ray to check for pneumonia. Total cost: $250.’
He’s got to write that down, along with the cost of the X-ray and painkillers and such. That way the insurance knows the patient owes the doctor for a cough treatment, not just a routine checkup.
If the doctor is careful and clear, the insurance will see he did right by her, and pay up. A doctor’s got overheads to meet, after all. Keeping good records and charging fair via the UB-04 form ensures the whole operation stays afloat.
3). Reduces claim denials.
The UB-04 lowers the number of bills insurance companies refuse by clearly showing the treatment, cost, and medical terms.
For example, imagine a man hospitalized with chest pain. Tests show two blocked heart arteries needing bypass surgery. Surgeons perform coronary artery bypass graft, or CABG. The hospital sends a UB-04 to the insurance company with codes for tests, surgery, drugs, and stay. The insurance folks understand CABG and medical terms on the standardized form, so they pay the claim.
4). Enables reimbursement through claim submission.
By reporting the specifics of each patient visit and the associated fees, the UB-04 form enables hospitals and physicians to receive payment for their services so they can keep the lights on, pay their staff, and continue helping the sick and injured. For healthcare organizations, reimbursement is lifeblood, and the unassuming UB-04 form provides transfusion.

5). Helps identify all healthcare professionals involved in a patient’s treatment.
The UB-04 is important because it lets the hospital tell the insurance company all the doctors, nurses, and staff that cared for the patient. That way, the insurance company knows exactly what they need to pay for. The form has boxes for the hospital to write the names and details of all the people involved in the patient’s treatment. So at the end of the stay, the insurance company can see the whole picture and reimburse the hospital properly. The hospital can then pay the staff accordingly. It’s a simple form that helps keep things clear and fair.
Who Uses the UB-04 Claim Form for Billing the Medical Services?
Institutional healthcare providers, such as hospitals, nursing facilities, dialysis centers, home health agencies, hospice providers, PRTFs, swing-bed facilities, all use the UB-04 claim form to bill inpatient and outpatient services and submit claims for reimbursement to insurance companies and other payers.
Let us detail down these providers who will use the UB-04 claim form for billing the healthcare services.
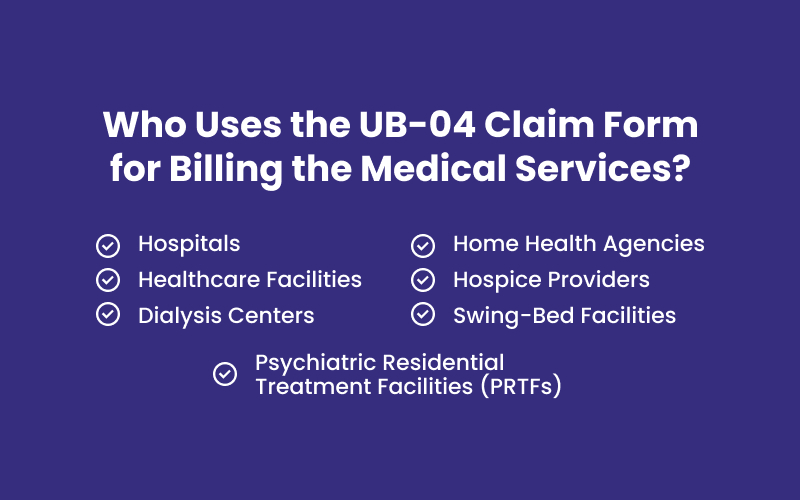
➜ Hospitals — General hospitals, children’s hospitals, and specialty hospitals all use the UB-04 form to bill for inpatient and outpatient services, including surgeries, diagnostic tests, and other medical treatments.
➜ Healthcare Facilities — Skilled nursing facilities (SNFs), long-term care facilities (LTCFs), and other nursing homes also use the UB-04 form to bill for daily care, therapy services, and other related healthcare services provided to residents.
➜ Dialysis Centers — Facilities offering hemodialysis and peritoneal dialysis services rely on the UB-04 claim form to bill for these specialized treatments.
➜ Home Health Agencies — Agencies providing in-home healthcare services, such as skilled nursing care, physical therapy, and occupational therapy, also use the UB-04 form to bill for these services.
➜ Hospice Providers — Organizations offering end-of-life care and support to terminally ill patients utilize the UB-04 form to bill for hospice services.
➜ Psychiatric Residential Treatment Facilities (PRTFs) — Facilities providing residential treatment for individuals with mental health conditions use the UB-04 form to bill for services such as therapy, medication management, and daily living support.
➜ Swing-Bed Facilities — Hospitals with designated swing beds that can be used for both acute and long-term care utilize the UB-04 form to bill for both types of services.
🔽🔽🔽
But Why Do These Specific Providers Use the UB-04 Form?
The UB-04 form was created by the National Uniform Billing Committee to meet the complex billing needs of institutional providers, as opposed to a simple claim form a solo doctor would use.
The UB-04 captures all the details the insurance companies need to process claims from facilities, like the dates the patient was admitted and discharged if they were hospitalized, or the specific date of an MRI if they just came in for an outpatient test.
So any healthcare provider that’s an “institutional” one – meaning they’re a facility with multiple doctors rather than just one – uses the UB-04 because it’s designed for their type of complex billing.
Click here to learn the difference between Institutional and Professional Billing Claims.
Where is the UB-04 Claim Form Used?
The UB-04 claim form plays a crucial role in the healthcare billing process, serving as the standardized format for institutional healthcare providers to submit claims for reimbursement to various entities, including:
- Commercial Insurance Companies
- Medicare and Medicaid
- Other Government Payers
- Workers’ Compensation Programs
- Self-Pay Patients
Commercial Insurance Companies
Private health insurance companies rely on the UB-04 form to process claims for services provided to their insured patients by institutional providers.
Medicare and Medicaid
These government programs utilize the UB-04 form for claims submitted by hospitals, nursing homes, and other institutional providers for services rendered to eligible beneficiaries.
Other Government Payers
UB-04 Claim Form is used by various state and federal government programs beyond Medicare and Medicaid for claims processing, including military healthcare programs, specific disease management programs, and more.
Workers’ Compensation Programs
When an employee is injured on the job, the UB-04 form is often used to submit claims for services provided by institutional healthcare facilities to the relevant workers’ compensation program.
Self-Pay Patients
Even for patients without health insurance, the UB-04 form can be used to document and bill for services rendered, helping the healthcare facility collect payment directly from the patient.
UB-04 Claim Form Instructions
The UB-04 form has a specific structure designed to efficiently capture and communicate billing information for institutional healthcare providers. Complete each section accurately to ensure smooth claim processing and timely reimbursement.
Here’s a detailed breakdown of how to fill it out:
| Form Locators (FL) | UB-04 Claim Form Field Explanation | Inpatient Requirement | Outpatient Requirement |
| 1 | Provider Name, Address & Phone NO ➤ Enter the full name and complete physical address of the provider submitting the claim. ➤ Include city, state, and ZIP+4 ➤ Ensure the name matches the NPI in FL56 in the UB-04 form. | Required | Required |
| 2 | Pay-To Name, Address & Phone NO ➤ Enter the provider’s name, address where payment should be mailed, and phone number. | Required | Required |
| 3a | Patient Control Number ➤ Enter the patient control number assigned by the provider. | Required | Required |
| 3b | Medical Record Number | Situational | Situational |
| 4 | Type of Bill Codes ➤ Enter the three-digit UB-04 claim form type of bill code, where the first digit identifies the facility type, the second classifies the care type, and the third shows the sequence. | Required | Required |
| 5 | Federal Tax Number ➤ Enter the provider’s federal tax number in the format XX-XXXXXXX. | Required | Required |
| 6 | Statement Covers Period ➤ Enter the beginning and ending dates of service in MMDDYYYY format. | Required | Required |
| 7 | Future Use | N/A | N/A |
| 8a | Patient ID ➤ Enter the patient identifier assigned by Security Health Plan, if different from the subscriber ID in FL60. | Required | Situational |
| 8b | Patient Demographics ➤ Enter the patient’s last name, first name, and middle initial. | Required | Required |
| 9 | Patient Address ➤ Enter the patient’s complete address, including street address, city, state, zip code, and country code. | Required | Required |
| 10 | Patient Birthdate ➤ Enter the patient’s birth date in MMDDYYYY format. | Required | Required |
⮟⮟⮟ Click here to reveal the complete 81 fields of the UB-04 Claim Form ⮟⮟⮟
| Form Locators (FL) | UB-04 Claim Form Field Explanation | Inpatient Requirement | Outpatient Requirement |
| 11 | Patient Sex ➤ Enter M for male, F for female, or U for unknown. | Required | Required |
| 12 | Admission Date ➤ Enter the admission date in MMDDYYYY format. | Required | Required, if applicable |
| 13 | Admission Hour ➤ Enter the admission hour in military time using two numeric characters. | Required | Required, if applicable |
| 14 | Type of Admission or Visit ➤ Enter the type of admission/visit using a single alphanumeric character. | Required | Required |
| 15 | Source of Admission ➤ Enter the source of admission using a single alphanumeric character. | Required | Required |
| 16 | Discharge Hour ➤ Enter the discharge hour in military time using two numeric characters. | Required | N/A |
| 17 | Patient Discharge Status ➤ Enter the patient’s discharge status using two numeric characters. | Required | Required |
| 18-28 | Condition Codes ➤ Enter two alphanumeric characters for each condition affecting claim processing. | Required, if applicable | Required, if applicable |
| 29 | Accident State ➤ Enter the two-letter state abbreviation where the accident occurred, for example, NY for New York. | Situational | Situational |
| 30 | Future Use | N/A | N/A |
| 31-34 | Occurrence Codes and Dates ➤ Enter two alphanumeric characters for each significant event related to the claim. ➤ Enter the date in MMDDYYYY format. | Required, if applicable | Required, if applicable |
| 35-36 | Occurrence Span Codes and Dates ➤ Enter two alphanumeric characters for each event related to claim payment. ➤ Enter the date range in MMDDYYYY format in each field. | Required, if applicable | Required, if applicable |
| 37 | Future Use | N/A | N/A |
| 38 | Responsible Party ➤ Enter the name and address of the responsible party. | Required, if applicable | Required, if applicable |
| 39-41 | Value Codes and Amounts ➤ Enter two alphanumeric characters for each data element required for claim processing and the corresponding dollar amounts or values. | Required, if applicable | Required, if applicable |
| 42 | Revenue Code ➤ Enter the appropriate revenue code for each healthcare service. | Required | Required |
| 43 | Revenue Code Description ➤ Enter a description or standard abbreviation for each revenue code. | Required | Required |
| 44 | HCPCS/Rates ➤ Enter the HCPCS code for ancillary services (outpatient) or the HIPPS / accommodation rate for inpatient claims. | Required, if applicable | Required, if applicable |
| 45 | Service Date ➤ Enter the date of service in MMDDYYYY format. | N/A | Required |
| 46 | Units of Service ➤ Enter the number of service units provided. | Required | Required |
| 47 | Total Charges (By Revenue Code) ➤ Enter the total charge per revenue code line. | Required | Required |
| 48 | Noncovered Charges ➤ Enter the total non-covered charge for each service line. | Required, if applicable | Required, if applicable |
| 49 | Future Use | N/A | N/A |
| 50 | Payer Identification (Name) ➤ Enter the name of each health plan expected to contribute to the payment (primary, secondary, and tertiary). | Required | Required |
| 51 | Health Plan Identification Number ➤ Enter the health plan ID for each payer listed in FL50 in the form. | Situational | Situational |
| 52 | Release of Info Certification ➤ Indicate whether the provider has a signed release form for each payer. | Required | Required |
| 53 | Assignment of Benefit Certification ➤ Showcase if the provider has authorization for direct payment from each payer. | Required | Required |
| 54 | Prior Payments ➤ Enter the prior payments received from each payer. | Required, if applicable | Required, if applicable |
| 55 | Estimated Amount Due ➤ Enter the estimated amount due from each payer. | Required | Required |
| 56 | Provider’s NPI ➤ Enter the NPI of the provider submitting the bill. | Required | Required |
| 57 | Other Provider IDs | Optional | Optional |
| 58 | Insured’s Name ➤ Enter the insured individual’s name as qualified by the payer. | Required | Required |
| 59 | Patient’s Relation to the Insured ➤ Enter the relationship code to the insured individual. | Required | Required |
| 60 | Insured’s Unique ID ➤ Enter the insured’s unique ID assigned by the payer. | Required | Required |
| 61 | Insured Group Name ➤ Enter the group or plan name for the insured’s coverage. | Situational | Situational |
| 62 | Insured Group Number ➤ Enter the group identification number assigned by the insurance company. | Situational | Situational |
| 63 | Treatment Authorization Codes ➤ Enter any authorization codes for the treatment covered by the bill for each payer. | Required, if applicable | Required, if applicable |
| 64 | Document Control Number (DCN) ➤ Enter the payer’s internal control number assigned to the bill. | Situational | Situational |
| 65 | Employer Name ➤ Enter the name of the employer providing health insurance for the insured individual. | Situational | Situational |
| 66 | Diagnosis/Procedure Code Qualifier ➤ Specify the ICD version used. | Required, if applicable | Required, if applicable |
| 67 | Principal and Other Diagnosis Code ➤ Enter the principal diagnosis code with the present on admission (POA) indicator. | Required | Required |
| 68 | Future Use | N/A | N/A |
| 69 | Admitting Diagnosis Code ➤ Enter the admission diagnosis code. | Required | Required |
| 70 | Patient’s Reason for Visit Code ➤ Enter the patient’s reason for visit at outpatient registration. | Situational | Situational |
| 71 | PPS Code ➤ Enter the DRG assigned to the claim based on the grouper software. | Situational | Situational |
| 72 | ECI (External Cause of Injury) ➤ Enter the external cause of injury code(s). | Situational | Situational |
| 73 | Future Use | N/A | N/A |
| 74 | Principal Procedure Code/Date ➤ Enter the principal procedure code, date, and up to five other procedure codes with corresponding dates. | Required, if applicable | Required, if applicable |
| 75 | Future Use | N/A | N/A |
| 76 | Attending Name/ID-Qualifier 1G ➤ Enter the attending provider’s name and NPI. | Required | Required |
| 77 | Operating ID ➤ Enter the operating provider’s name and NPI. | Situational | Situational |
| 78-79 | Other ID ➤ Enter the names and NPIs of other providers involved. | Situational | Situational |
| 80 | Remarks ➤ Enter any additional information necessary for claim adjudication. | Situational | Situational |
| 81 | CC Codes ➤ Enter overflow or additional codes related to field locators or externally maintained codes approved by the NUBC. | Not Required | Not Required |
FAQs About UB-04 Claim Form
What is the difference between CMS 1500 and UB-04 claim forms?
The key difference lies in the types of providers using each form. CMS 1500 (HCFA-1500) is used by physicians and other individual healthcare providers to bill for their professional services. And UB-04 is used by institutional facilities to bill for services provided within the facility.
How many boxes or fields, blocks, or form locators (FLs) are in the UB-04 claim form?
The UB-04 claim form has 81 individual fields, boxes, or blocks, also known as Form Locators (FLs). Each FL has a specific purpose and requires unique information to be filled in for accurate claim processing. Understanding each FL is crucial to ensure smooth reimbursement.
How to get UB-04 form from hospital?
Hospitals typically don’t provide the UB-04 form directly to patients. The UB-04 form is used by the hospital itself to bill insurance companies for services provided to patients.
However, you can get the UB-04 form in the following ways:
- Download it online: You can find blank UB-04 forms on the websites of healthcare organizations and government agencies.
- Contact your insurance company: Some insurance companies also provide pre-filled UB-04 forms for their members.
- Request it from the hospital’s billing department: While not common, you can contact the hospital’s billing department and inquire about obtaining a copy of your UB-04 form.
Do You Find It Hectic To Fill and Complete The UB-04 Form? Get Immediate Help Here!
In the hectic world of healthcare, claim filing is an unwanted chore. Our medical billing service lifts the burden of paperwork from your facility so you can do what you do best, provide top quality care.
We grasp the complexities of the UB-04 form and insurance procedures to guarantee your claims are submitted correctly the first time. Our experienced staff treats each claim with care and urgency to accelerate your reimbursement.
Why deal with the hassle yourself? Our company’s billing service allows you to offload the responsibility and headaches that come with claim filing. Choose us as your partner in healthcare administration.