BellMedEx Medical Revenue Cycle Management Service
Request Free RCM Consultancy
Importance of Choosing BellMedEx Revenue Cycle Management Service in Medical Billing

Managing a medical practice’s finances is complex. Between evolving regulations, strict insurance policies, and patients with expectations higher than Mt. Everest – it’s a recipe for revenue leakage, cash flow disaster, and operational chaos.
Luckily, the medical revenue cycle management (RCM) experts at BellMedEx can restore your practice to full financial health. Our certified coders ensure accurate billing and coding to stop revenue leakage. Our enrollment specialists secure contracts with top commercial payers to expand your patient pool. And our billing experts work diligently to collect every dollar your practice earns.
So don’t let medical finances frustrate you. BellMedEx Medical Revenue Service has the cure for what ails your practice’s finances. Call today to experience how we align a provider’s whole revenue cycle process to maximize collections while delighting patients.
You are a professional in your field.
But are you getting paid like one?
Claim your FREE practice audit to learn how!
BellMedEx offers revenue cycle care, with billing at its core
Our unique approach to medical billing is how BellMedEx RCM Service delivers measurable improvements to the revenue cycle process. The SmartClaim system we developed in-house analyzes billing codes and clinical documentation to catch issues before claim submission. This technology achieves first-time acceptance rates upwards of 98%, putting money back in our providers’ pockets faster.


Achieve revenue cycle success via BellMedEx coding excellence
BellMedEx’s medical revenue service boosts revenue cycles through expert medical coding. Our acclaimed BellCoding technology reviews medical charts and identifies high-value codes. Our coders, armed with CPC certifications, then examine each chart to find revenue escalation opportunities algorithms miss. Through this man-machine symbiosis, BellMedEx delivers an RCM solution that promises more revenue for your healthcare facility.
Optimize your revenue via BellMedEx’s audit and insight
Our audit specialists utilize the BellMedEx Revenue Integrity process to analyze your current revenue cycle, uncovering exactly where coding and billing improvements will have the biggest impact. Our billing consultants then design targeted solutions to resolve those defects. We treat your revenue cycle as a whole and prescribe the best healthcare revenue cycle management remedies to make it stronger.

RCM ROI CASE STUDY
Up To 30% Revenue Increase In Next 12 Months With BellMedEx's Medical Revenue Service (Case Study)
| In-House Billing | BellMedEx RCM | Results | |
|---|---|---|---|
| Charges (on average) | $142,000.00 | $142,000.00 | |
| Gross Collection Rate (GCR) | $60,000 (42%) | $77,000 (54%) | 12% Increase in Gross Collection Rate |
| Billing Costs | $6,000 | $4,000 | $2,000 Decrease in monthly cost of RCM service |
$197,000
Yearly Net Benefit
(monthly gross collection * 12 months)
≈ 30%
Overall collection increase
The actual results may vary depending on various factors such as the size of the facility, the number of providers, the type of services offered, the payer mix, the billing efficiency, and the market conditions.
End-to-End RCM Service Features by BellMedEx
You have nothing to lose and everything to gain with BellMedEx Medical Revenue Cycle Management features. This means our healthcare RCM service is the partner you can trust for your revenue cycle success.
Charge Entry Feature
- Claim creation, validation, and transmission
- Entering valid super-bill information
- Claim approval confirmation
- Claim status tracking
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Remittance Processing Feature
- Processing of payments from the payers
- Processing of adjustments and denials
- Reconciling payments to the provider’s claims
Insurance Follow-Up Feature
- Following up with payers for unpaid claims
- Following up with payers for underpaid claims
- Contact payers on a provider’s behalf
- Negotiating and resolving claim disputes
KPI Reporting & Analytics
- Monitors your key performance indicators
- Analyzes days in accounts receivable
- Analyzes claim denial rate and collection rate
- Comprehensive and customizable reports
- Advanced data visualization tools
Patient Collections Feature
- Collecting patient payments
- Managing initial statement + final notice
- Sending clean bills and reminders to patients
- Convenient payment options for patients
A/R Management Feature
- Reduces the aging of outstanding A/R
- A/R workflow optimization
- Claim approval confirmation
- Collecting A/R collections from the payers and patients
Coding and Documentation
- Coding provider’s services compliantly
- Using the latest coding standards and guidelines
- Capturing relevant details that support a provider’s claims
- Justifying a provider’s reimbursement for their services
- Performing medical bill audits
Charge Capture Feature
- Capturing and validating the service charges
- Leveraging charge sheets and EHRs
- Ensuring charges are consistent with coding and documentation
- Reconciling your charges with your claims
- Reconciling charges with your contractual agreements with the payers
Contract Management
- Managing contractual agreements with the payers
- Determining how much you get paid for your services
- Reviewing and negotiating your contracts
- Monitoring the contracts’ compliance
- Analyzing the contract performance
- Using metrics like contract yield and case mix index (CMI)
Let BellMedEx RCM Service seal cracks in your revenue cycle...
We identify opportunities to boost your revenue through enhanced billing, coding, denial management and more.
- Claims Management
- Denial Prevention
- AR Optimization
- Improved Collections
BellMedEx RCM Medical Billing Has Got The Solutions For Providers' Revenue Growth
Poor Cash Flow
Providers struggle with maintaining a steady and predictable cash flow due to various factors such as bad debt and underpayments.
Mishandled A/R
Providers face challenges in managing their accounts receivable (A/R) due to the complexity and variability of the process.
Misaligned Payer Compatibility
Providers struggle complying with multiple payers, as well as different claim types, like fee-for-service, value-based, and capitated.
High Denial Rates
Providers experience is a high rate of denials from payers, that give negative impact to their revenue and also to their cash flow.
More Admin Workload
Denials reduce the provider’s revenue collection and increase their workload as they have to appeal and resubmit the claims.
Unsatisfied Patients
Patients are becoming more empowered consumers of healthcare services, so providers find it hard to ensure patient satisfaction.
Complicated Patient Management
Providers struggle with the increasing patient financial responsibility due to high deductible health plans (HDHPs) and self-pay patients.
Better Cash Flow
Our med RCM service reduces the bad debt and underpayments by ensuring accurate and timely claim submission and follow-up.
Managed A/R
Our healthcare RCM solution provides visibility into A/R performance, such as days in A/R, A/R aging, and A/R turnover.
Aligned Payer Compatibility
Our flexible and scalable RCM platform adapts to the changing payer requirements and maximizes provider’s reimbursements.
High Recovery Rates
Our proactive and preventive approach resolves the root causes of denials to boost denial recovery rates and revenue integrity.
Automated Process
Our RCM experts and EHR platform automate the manual work and perform claim submission with utmost accuracy.
Satisfied Patients
Our RCM service offers a patient-centric platform to improve the patient-payer relationship via telehealth features.
Automated Patient Management
Our medical billing platform automatically estimates and communicates the patient’s out-of-pocket costs before the service.
Poor Cash Flow
Providers struggle with maintaining a steady and predictable cash flow due to various factors such as bad debt and underpayments.
Better Cash Flow
Our med RCM service reduces the bad debt and underpayments by ensuring accurate and timely claim submission and follow-up.
Mishandled A/R
Providers face challenges in managing their accounts receivable (A/R) due to the complexity and variability of the process.
Managed A/R
Our healthcare RCM solution provides visibility into A/R performance, such as days in A/R, A/R aging, and A/R turnover.
Misaligned Payer Compatibility
Providers struggle complying with multiple payers, as well as different claim types, like fee-for-service, value-based, and capitated.
Aligned Payer Compatibility
Providers face challenges in managing their accounts receivable (A/R) due to the complexity and variability of the process.
High Denial Rates
Providers experience a high rate of denials from payers, which negatively impact their revenue and cash flow.
High Recovery Rates
Our proactive and preventive approach resolves the root causes of denials to boost denial recovery rates and revenue integrity.
More Admin Workload
Denials reduce the provider’s revenue collection and increase their workload as they have to appeal and resubmit the claims.
Automated Process
Our RCM experts and EHR platform automate the manual work and perform claim submission with 100% accuracy.
Unsatisfied Patients
Patients are becoming more empowered consumers of healthcare services, so providers find it hard to ensure patient satisfaction.
Satisfied Patients
Our RCM service offers a patient-centric platform to improve the patient-payer relationship via telehealth/telemedicine features.
Complicated Patient Management
Providers struggle with the increasing patient financial responsibility due to high deductible health plans (HDHPs) and self-pay patients.
Automated Patient Management
Our medical billing platform automatically estimates and communicates the patient’s out-of-pocket costs before the service.
REPORTING & ANALYTICS FEATURES
Choose BellMedEx RCM Billing Company For Complete RCM Reporting
Data Insights
See the key metrics and trends of the revenue billing process in a comprehensive and interactive analytics dashboard. You can compare your performance with industry benchmarks and identify areas for improvement.
Quick Feedback
Communicate with our RCM experts, your patients, and the insurance payers instantly through the integrated chat system. You can ask questions, share feedback, and resolve issues in real time.
Detailed Reports
Drill down into the details of your revenue cycle with our customizable and granular reports. You can filter, sort, and export your medical billing data according to your needs and preferences.
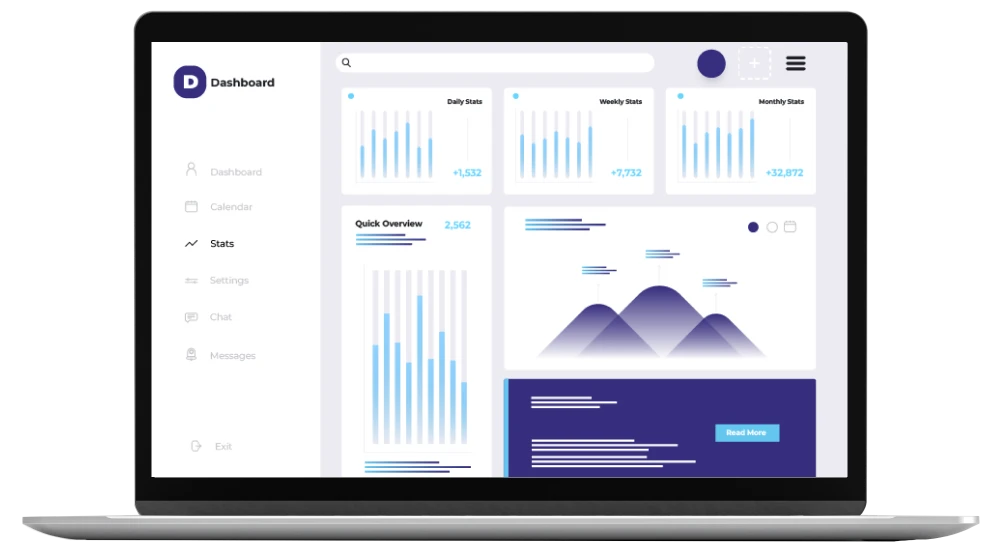

Multi-Specialty Support
Manage multiple facilities and locations with our RCM reporting dashboard. You can view and compare the data of different sites and groups in one place. Dedicated dashboard for each specialty.
Data Security
You can rest assured that your data is safe and secure. We use the latest encryption and authentication technologies to protect your data from unauthorized access and breaches.
Data Integration
You can integrate your data with other systems and platforms with BellMedEx’s RCM reporting dashboard. We support various formats and standards to ensure seamless data exchange and interoperability.
Testimonials

Dr. Julia Will***
Licensed Professional Counselor
I would like to send out a heartfelt appreciation for all of your hard work in helping my Health Counselling clinic take care of our billing and credentialing needs. You have made my job as a practice owner much easier.

Dr. Gennaya Matt***
Plastic Surgeon
We are more than satisfied with BellMedEx and would highly recommend them to anyone searching for an efficient billing company. Working with BellMedEx has felt effortless and we are vastly thankful for their services.

Dr. Mike Lan***
Internal Specialist Medicine
BellMedEx has been a phenomenal asset to our company. Assisting with billing, credentialing and enrollment, BellMedex has been consistently reliable from the first day of our relationship.

Dr. Belen Bur***
Psychiatrist
Tiida B***
Catonsville, Maryland
Our medical facility has been working with BellMedEx for about 2 years now and we are very pleased with their services. BellMedEx Medical Billing is a great company for billing needs. The customer support is great.
Frequently Asked Questions
Revenue cycle management is the process of managing the financial aspects of a healthcare provider’s or facility’s operations. It involves billing, coding, collecting, and reconciling payments from patients and insurance companies.
RCM services can help you improve your cash flow, reduce administrative costs, increase patient satisfaction, and comply with regulatory requirements.
We have a robust and proactive system to handle claim denials and appeals. We first monitor and analyze the reasons for claim rejections and denials. Then, correct and resubmit the claims as soon as possible. We also follow up with the payers and negotiate on your behalf to get the maximum reimbursement. We keep the provider informed of the status and outcome of the claim denials and appeals.
We charge for our RCM services based on a percentage of your collections. This means that you only pay us when you get paid by the payers and patients. We do not charge any upfront fees, hidden fees, or long-term contracts. We believe that this pricing model is fair and transparent, and it aligns our interests with yours.
We take the security and privacy of your data very seriously. We comply with all the relevant laws and regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR). We use encryption, firewalls, backups, and other measures to protect your data from unauthorized access, loss, or damage.
We measure and improve our RCM performance using various metrics and indicators, such as:
Days in accounts receivable (DAR): the average number of days it takes to collect the payments from the payers and patients
Claim acceptance rate: the percentage of claims that are accepted by the payers without any errors or rejections
Denial rate: the percentage of claims that are denied by the payers for various reasons
Collection rate: the percentage of the total amount billed that is collected from the payers and patients
Net collection ratio (NCR): the percentage of the total amount allowed by the payers that is collected from the payers and patients
Our medical billing company has the expertise, technology, and resources to handle all aspects of your RCM process. We can help you with:
- Coding and submitting accurate claims to payers
- Tracking and following up on claim status and denials
- Posting and reconciling payments from payers and patients
- Managing patient accounts and statements
- Providing reports and analytics on your financial performance
You’ve Won a Free Audit!
Claim your prize now and boost your revenue cycle.

