Whether you are a therapist wishing to grow your practice or need therapeutic services, understanding the ins and outs of insurance credentialing proves vital. As the demand for therapy services continues to rise, Therapists face the issues of navigating the challenging waters of insurance credentialing. In this blog, we’ll explore how this process can shape the landscape of therapeutic practice.
Understanding Insurance Credentialing
Insurance credentialing, also known as Provider Enrollment, is a process of partnering with a health insurance network and becoming a member of their provider panel. Insurance companies examine the Therapist’s educational history, professional experience, and training to see if he meets the internal requirements for working as an in-network provider. The procedure is making an application request, completing the Credentialing process, presenting the necessary documents, and signing the contract after being approved by the Credentialing Committee.
The Insurance Credentialing for therapists consists of two phases:
- Credentialing
- Contracting
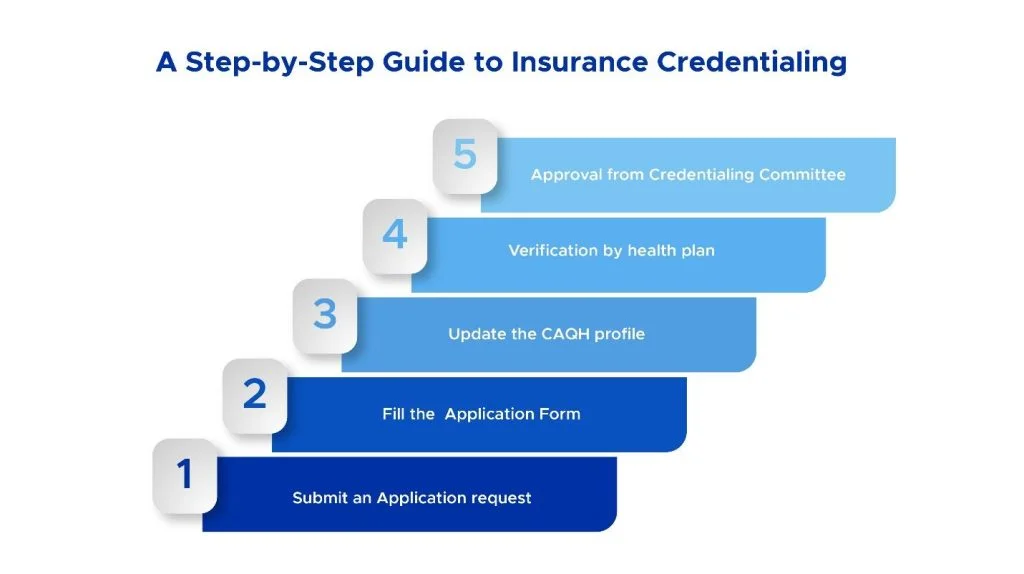
Phase #1 Steps: Credentialing
1). The first step is to contact the health plan and request an application. Inquire with the network provider’s services department about their credentialing process and request an application.
2). The second step is to complete the Application by stating all requested information, signing and dating it, and attaching copies of all relevant papers.
3). The following step is to update the CAQH profile with all the necessary information, such as the practice address. Provide all required documentation, including a license, insurance, and a copy of your board certification.
4). When a health plan receives an application, the Therapist’s credentials are thoroughly verified to ensure they fit its credentialing requirements.
5). After verification, the credentialing file is delivered to the Credentialing Committee for approval.
Phase #2 Steps: Contracting
After completing the credentialing process, the network takes 30-45 days for contracting.
1). In the Contracting phase of enrollment, the health plan goes over the contract text, reimbursement rates, and all the specifics and duties of the Therapist.
2). The following step is to sign the agreement.
3). The provider can negotiate at this point on reimbursement rates if standard reimbursement rates don’t meet the expectations.
Importance of Insurance Credentialing for Therapists
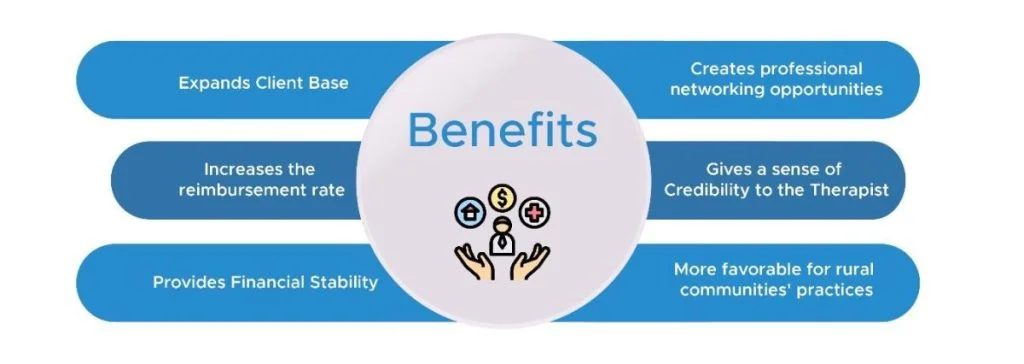
Therapists need insurance credentialing to bill insurance companies, which can help patients afford treatment. Here are some more benefits:
Expands Client Base
Insurance credentialing allows therapists to attract more clients who accept their insurance. They can also benefit from the insurance company’s marketing efforts, as it can list therapists in its preferred provider directory.
Increases the Reimbursement Rate
Therapists can negotiate with insurance companies for higher fees, especially if they specialize in elevated-demand niches. A higher Reimbursement rate means a therapist earns more income.
Gives a Sense of Credibility to the Therapist
When insurance companies credential a therapist, it implies that the therapist can now exhibit his skills and competence to potential clients who may trust the vetting procedure of the insurance business. Connecting with a well-known insurance brand can also help improve reputation and exposure.
Provides Financial Stability
Insurance Credentialing provides a stable and reliable stream of income, which may be more predictable and consistent than clients on private pay. This can assist therapists in budgeting and managing their cash flow.
Creates Professional Networking Opportunities
Professional networking opportunities could occur when therapists are linked with other providers on the same insurance panel or who recommend clients to them. This can assist therapists in developing relationships and collaborations to improve their practice and reputation.
Favors Rural Communities’ Practices
Insurance credentialing enables therapists to treat clients with restricted access to mental health care due to geographic or economic constraints. They can fill a market gap because fewer therapists may accept insurance in rural locations.
Credentialing and Contracting Procedural Checklist
- Form a business entity to practice (LLC, S-Corp, PC, etc.) and receive a tax ID.
- Acquire professional liability insurance.
- Obtain an NPI number for the individual (type 1) and the business organization (type 2).
- Be fully licensed in the state where services are to be provided (including prescriptive authorization).
- Establish and maintain a CAQH profile.
- Prepare the practice location.
- Determine which insurance networks you want to join.
Credentialing Procedure Duration
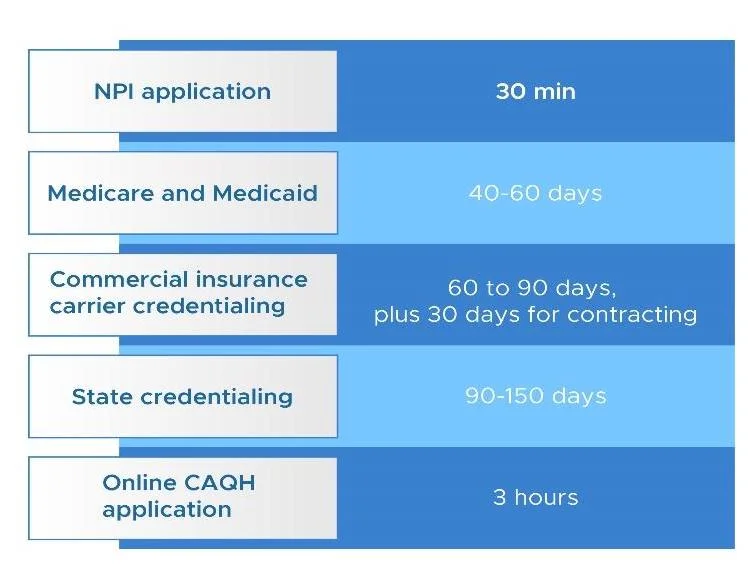
The length of the process varies depending on the company or agency you are dealing with. The approval time can be anticipated in general as follows:
| Credentialing Process Type | Duration |
| NPI application | 30 minutes |
| Medicare and Medicaid | 40 to 60 days |
| Commercial insurance carrier credentialing | 60 to 90 days + 30 days for contracting |
| State credentialing | 90 to 150 days |
| Online CAQH application | 180 minutes |
Common Provider Enrollment Errors to Avoid
Here are the three most common provider enrollment errors to avoid, so you can ensure a smooth and successful enrollment process.
Failure to Provide Complete Information
The therapist should offer detailed information about his history and current medical practices so that the insurance company may determine his eligibility to be placed on the provider list. All information concerning the address, contact number, copies of the operating license, a thorough profile of the patients, legal difficulties (if any), and other business-related papers must be submitted on time and with a valid signature of the therapist. Failure to provide these details may cause a delay in the Application’s processing.
Not Starting Early
The provider credentialing process should start when the therapist applies for an employment contract. Surprisingly, you must patiently wait up to 6-8 months for all the requirements to get over. The worst-case scenario occurs when the therapist has a full schedule yet is not credentialed. When this happens, the therapist is forced to reschedule all the patients. So, starting the insurance credentialing process three months before setting up the practice is advisable.
No Follow-Up
It takes almost 12 months for credentialing approval and gets included in the provider network. So, the therapist should have regular follow-ups and be updated on the status of his Application. When there is no follow-up, the therapist is unaware of the problems; by the time he becomes mindful of them, it may be too late. Proactively checking the application progress is the best way to keep ahead of the competition.
Best Practices for Successful Insurance Credentialing
Every therapist must adopt these best practices for successful insurance credentialing to ensure that they are able to provide their services to as many patients as possible.
Conduct Your Research and Make a List
Every insurance company has a unique set of processes and obstacles to offer. That is why a therapist needs to make a list and determine the ones he wants to be credentialed with.
Important Things to Have Before Starting the Journey
- National Provider Identifier (NPI) is readily available
- Current Licence in the state, a therapist is practicing
- Proof of Liability insurance
- Current resume or CV with employment history for the previous five years.
- At least three professional references
- Evidence of any special credentials or qualifications
Complete Your CAQH Before Starting the Credentialing Process
CAQH will have the upload or fax the documents required for credential verification. Once registered, the Therapist will be given a CAQH identifying number, which insurance companies may request. Maintain your CAQH profile with quarterly attestations and document updates if you renew licenses or malpractice insurance.
Be Willing to Invest Time
Make yourself ready to accept the fact that this will take time. From the time the therapist begins the credentialing process until insurance companies reimburse him, it will take 2 to 6 months.
Maintain All the Forms
You need to make copies of all the application forms, contract forms, and enrollment letters.
Know About the Latest Provider Enrollment Credentialing Rules
The therapist should be aware of all the newest provider credentialing enrollment rules in his country and ensure that he follows them strictly to avoid delays in the process.
Bottom Line
Insurance credentialing is vital for therapists interested in working with insurance companies. It provides prospects such as an expanded client base, more reliability, and financial stability. Enrolling in insurance panels is a difficult process. However, the rewards may outweigh the initial efforts. Therapists can establish themselves as reputable providers in the health industry by taking the appropriate procedures.