HEALTHCARE FUSION EDI SOFTWARE
A fusion of EDI and Healthcare Billing for practices that want Speedy Rewards!
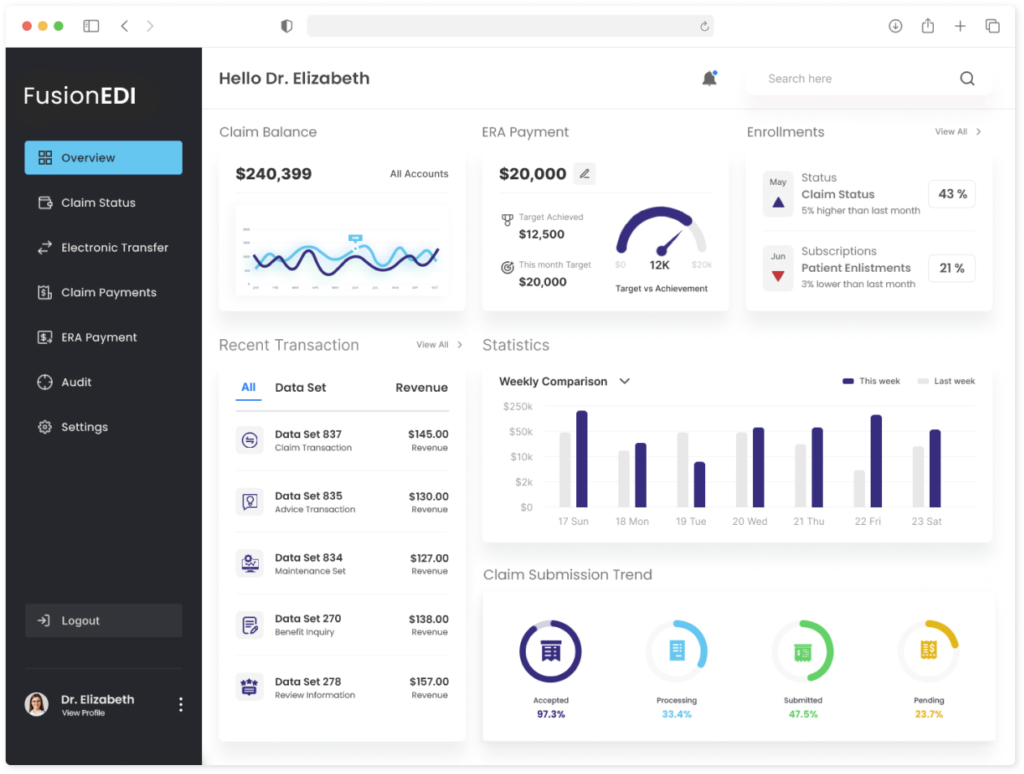
FusionEDI® is a healthcare clearinghouse EDI software for an ‘instant’ transmission of claims with absolute accuracy. Our scalable medical billing EDI solution scrubs claims, resolves denials, and verifies patient eligibility for a better medical revenue cash flow.

HEALTH INSTITUTE EDI SOFTWARE FEATURES
The No.1 Solution For The Billing Evolution
The billing landscape is changing fast, and you need a value-added network (VAN) that can adapt and grow with you. That’s why we created FusionEDI, a medical clearinghouse software that clears the way for your claims to get paid. Enjoy the benefits of EDI and billing in one powerful platform.
Claim Quality Assurance
The claim quality assurance process a.k.a claim scrubbing ensures that your claims are error-free & processed smoothly by the payers, with advanced features such as coding, charge posting, CTA code, and diagnosis code submission.

Data Format Alignment
Our EDI software transforms any non-standard data into standard data formats like 835/837 data files, which are electronically transferred into the payer’s adjudication system, ensuring faster reimbursement for your medical services.

Instant Claim Submission
Our clearinghouse software swiftly sends electronic claims to the insurance carriers. This helps medical facilities slash the hassle, dodge the errors, and pump up their cash flow. Lean on us to handle your claims with flair and commitment.

Get Started for Free in 3 Easy Steps
It’s free to use and has no hidden fees.
Step 1
Reach Out to Us
We are all ears. Send us an email or ring us up, and let us know about your practice and the medical billing software you have.
Step 2
Get FusionEDI Set UP
Our expert will configure FusionEDI clearinghouse software and make it fit like a glove with your medical billing software.
Step 3
Enjoy Fast Claims
FusionEDI will now start acting as a bridge between you and the payer, and ensure you get your fair share of the pie.
Step 1
Reach Out to Us
We are all ears Shoot us on email or ring us up, and let us know about your practice and the medical billing software you have.
Step 2
Get FusionEDI Set Up
Our expert will configure FusionEDI clearinghouse software and make it fit like a glove with your medical billing software.
Step 1
Enjoy Fast Claims
FusionEDI will now start acting as a bridge between you and the payer, and ensure you get your fair share of the pie.
WHAT WE OFFER
More Features, More Efficiency, and More Profitability.

Claim polisher
Cleanses & polishes claim data before sending it to payers, dodging penalties and denials.

Claim auditor
Gives feedback on the quality of claims, making sure all required fields are filled and no cracks are found.

Claim accelerator
Accelerates the claim processing cycle, resulting in faster payments and smoother cash flow for the provider.

Payment automator
Enables automatic posting of payments to patient accounts, minimizing errors and easing reconciliation.

Eligibility checker
Verifies the patient’s insurance coverage before the service is rendered, avoiding eligibility-related rejections.

Billing analyzer
Offers valuable insights into billing trends, patterns, issues and opportunities, supporting wise decision making.
Medical EDI Solutions
Clear the way for Better Healthcare with our Clearinghouse Solutions.
If you’re sick and tired of dealing with messy healthcare bills and claims, you need a dose of our clearinghouse solutions. From checking your patients’ coverage to getting paid faster, our medical clearinghouse software does it all. Try FusionEDI today and see the difference!
Fast Claim Submission
Instant Eligibility Check
Seamless Integration
Claim Quality Control
HIPAA Compliant Electronic Data Exchanges
The Next Generation Of Electronic Data Transfers In Healthcare
FusionEDI is powerful software that can handle various data types that are vital for the healthcare industry. Whether you need to submit, process, receive, or verify healthcare data, FusionEDI can do it all for you electronically. Here are some of the data types that FusionEDI supports:
Retail Pharmacy Claim
Submit and Process retail pharmacy claims electronically. This will save you time and money , and reduce errors and rejections.
EDI 835
Receive and process payments and remittance advice electronically. This will help you reconcile your accounts, track revenue, and manage denials.
EDI 270
Inquire and verify eligibility and benefits of subscriber electronically. This helps you avoid unnecessary claims denials and verify coverage details.
EDI 277
Receive and process the notifications about status of previously submitted EDI 837 claim electronically. This help you monitor the progress of your claims.
EDI 837
Submit and process healthcare claims and encounters electronically. This will improve your cash flow, compliance, and accuracy.
EDI 834
Enroll and manage members in a healthcare benefit plan electronically. This will streamline your enrollment process and reduce administrative costs.
EDI 271
Receive and process the responses to inquiries about the eligibility and benefits of subscriber electronically. This will help to understand the plan limitations.
EDI 278
Request and receive authorization for healthcare service electronically. This helps to ensure compliance with plan policies, and avoid claim rejections.
- Easy registration
- Access 24/7
- Specialty specific
Free Today, Premium All The Way.
Let's Get Started!
You have nothing to lose and everything to gain with our healthcare clearinghouse software. Contact us today for free access and discover how premium features can boost your efficiency and profitability.
