An efficient revenue cycle management flowchart helps submit accurate claims and improves cash flow.
Now, your revenue cycle management practices should be proactive rather than reactive to submit claims accurately. Implementing aggressive strategy and planning in advance is crucial to avoid financial losses and overcome any setbacks.
Moreover, your practice can lose a good fortune due to poor medical billing practices. It’s essential to note that a well-organized Revenue Cycle Management ( RCM) performs efficiently and has close to minimal denials and streamlined end-to-end claim denial management.
Steps to an Efficient Healthcare Revenue Cycle Management Flowchart
Navigating healthcare revenue cycle management (RCM) is no small task and requires attention to detail. Additionally, efficient healthcare revenue cycle management offers the potential to cut administrative costs while boosting revenue dramatically.
The key to a successful RCM flowchart lies in a comprehensive and robust approach that efficiently handles all the core tasks, from patient registration to coding and payment collection.
Streamlining Patient Registration
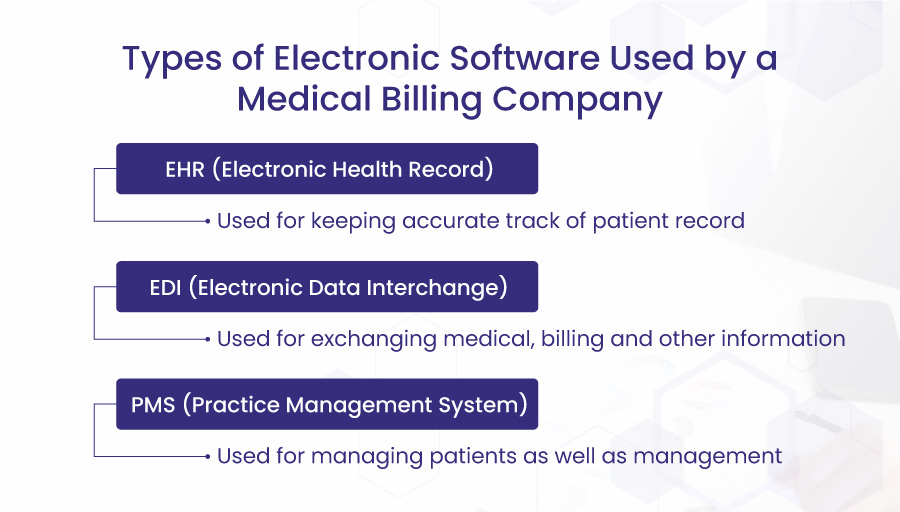
Patient registration is the primary step toward successful revenue cycle management. Therefore, the process should be as swift and smooth as possible. In this regard, utilizing practice management software and patient portals can significantly elevate operational and clinical productivity.
This step involves taking patient information required for medical records. This includes the overall demographics, contact, diagnosis, current medication, past history, etc. This information is vital to the patient’s future care services.
Leading RCM companies use innovative strategies to exceed the traditional cost and bottom-line growth targets. Bell MedEx leverages all the progressive strategies and tactics to lower billing costs and use practice management software.
Confirming Eligibility Verification
Eligibility verification is one of the most important steps in revenue cycle management. This process involves an outside party- the insurance company.
Patient insurance eligibility verification is essential to understand how much the insurance company will pay for the service provided. This would allow the provider to inform the patient upfront about the co-pay if any. It is recommended to confirm the patient’s insurance coverage, eligibility, and benefits to increase the chances of steady cash flow and avoid denials.
In case of no prior eligibility verification, the provider might face financial loss. For example, if the services are provided, the payer does not verify and the patient cannot afford the treatment. The provider will be the one to bear the expenses.
So ensuring eligibility verification before providing services is compulsory for your practice’s long-term financial health. Medical verification also includes policy carrier, policy status, plan type, age covered, co-pay information, family details, pre-authorization, claim submission, and more.
Medical practices must verify patients’ eligibility and benefits through Electronic Health Records (EHR) software before delivering healthcare services.
Bell MedEx ensures an efficient electronic health record software performance to ease practices and their patients. Providing patients with a comprehensive understanding of their coverage status can expedite bill clearance, reduce claim denial rates, and improve RCM.
Ensuring Accurate Data Entry
Accuracy in data entry precedes accurate claims submission. Inaccuracy in data entry leads to false billing and coding which ultimately results in lost revenue or slow revenue collection due to denied claims.
Once the data is submitted accurately it saves you from denied claims and lowers billing costs. Health insurance claim denials are on the rise and according to a survey, the denial rate is between 10%-20% which increases your billing costs and lowers overall practice efficiency.
Proper data entry is crucial to confirm patient identities and associate the correct information with the right individual. This precision is paramount for reducing medical billing errors and enhancing proficiency.
Securing Authorizations
Securing prior authorization for a service yet to be provided is crucial for steady workflow and minimum AR cycles.
Authorization refers to getting beforehand approval from the insurance company as to whether the service or treatment will be paid or not. If your practice fails to secure authorization it will lead to extra hassle, time, and cost.
Before the treatment begins, practices need to make sure whether the services require prior authorizations. Neglecting this step often results in a less-than-ideal patient experience. Properly managed authorizations enhance workflow efficiency and revenue cycle management.
Safeguarding Patient Information
Maintaining a smooth and pleasant patient encounter is vital to a great patient-provider relationship and overall revenue cycle management experience. For a smooth and efficient patient experience, it’s necessary to safeguard patient information and offer effective customer support.
According to a survey by Forbes, 60% of Americans have reported negative healthcare experiences in terms of longer wait times and delayed response. Moreover, safeguarding patient information is mandatory to avoid a breach of trust between the patient and the provider
Additionally, accurate coding and medical billing hinge on the quality of information stored in patient records. Regular updates in line with regulatory changes and meticulous workflow examination can help avoid costly compliance errors and provide opportunities to refine the patient experience.
An open communication between the patient and the provider is the key to providing a great patient experience.
Implementing Appropriate Charge Posting
In a successful RCM flowchart, proper charge posting is crucial. Providers must post claims to the correct payer to facilitate speedy reimbursements.
Clear, accurate, and comprehensive documentation of services provided, patient details, and insurance plans accelerate payment receipts. If the documentation or charge posting is incorrect it will delay your claim submission and hence payment collection.
In the series of efficient RCM steps, appropriate charge posting enables efficiency, top-notch services, and patient experience. The providers use electronic formats such as electronic health records (EHRs) to record the diagnosis, symptoms, and services provided to the insurance company.
According to recent research, 77% of providers say that it takes more than a month to collect payment and it all comes down to accurate and appropriate charge posting. Therefore, charge posting is a central protocol for an increased first-pass rate and overall billing and RCM.
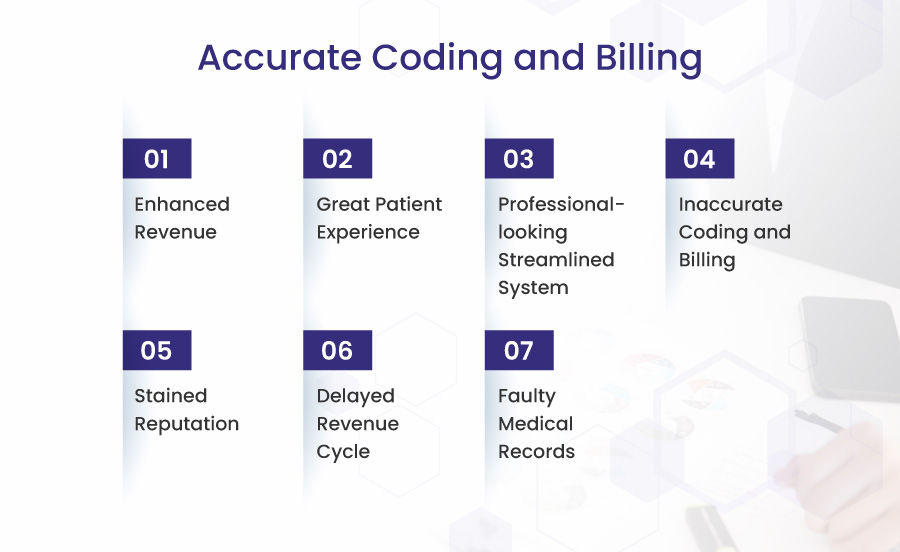
Maintaining Accurate Coding and Billing
Coding and billing is the back-end process of the revenue cycle management flowchart. In this step of the process, the correct billing is prepared and then claimed to the insurance company and to the patient as well if there’s a co-pay.
Coding and billing errors disturb the whole cycle of revenue collection therefore, proper attention and accuracy is compulsory for a steady workflow and cash inflow. Around 80% of medical bills have errors due to upcoding, unbundling, and other relevant errors.
These errors make your practice vulnerable to stained reputation and faulty record-making. Moreover, such errors defy the medical research data so it has huge negative implications for healthcare records.
Correct coding is the backbone of an error-less billing and revenue cycle. Coding of procedures and diagnosis should be done according to the International Classification of Diseases (ICD).
Mastering Management of Claims
Claims management is a complex, multi-step process. Eligibility verification, adherence to rules, and accurate coding combine together to determine if a claim is fully paid, partially paid, or denied. Lost revenue in denied claims is quite distressing as it costs you a lot of time and extra work hours.
Therefore, addressing the factors behind the denial should be the ultimate priority to combat the issue in its roots. In case of denial, practices must identify the underlying issues and assess whether reworking the claim is worth the time and cost.
Various RCM tools can automate status requests, providing valuable insight into potential claim denials, boosting productivity, and elevating reimbursements.
Bellmedex caters to end-to-end claims denial management and follows up on revenue cycle management with utmost efficiency.
Payer Contract Management
Once the claims are submitted the payer party takes some time to analyze and manage the terms. For a dispute-free contract, the terms and conditions must be targeted right from the start. An upfront settlement of the contract enables your practice to smoothly carry out all the steps of the revenue cycle management flowchart.
If there’s no payer contract it can lead to severe consequences in terms of changed payer policies and hence claim denial. To make contract management easier and effortless, the contract must be strategized and optimized with effective negotiations. Not just contract but a proper follow-up is also essential for a smooth and steady revenue cycle management flowchart.
Excelling at Billing and Collections
The final step in a well-rounded RCM flowchart is accurate patient billing. Excelling at billing and collections is only possible with accurate coding, payer management, addressing claims, and all of the above-mentioned steps. If any of the steps is missing it will lead to delayed claims and eventually slow revenue collection. Addressing delayed claims will ultimately result in increased billing costs, added load, and non-clinical burden.
To avoid non-clinical burdens, outsourcing your billing is more efficient, and practical, and makes you laser-focused on your core task- providing care. Bellemedex is here to do just that and more when it comes to efficient revenue cycle management.
The right RCM solution can streamline this process, but choosing a reputable provider is essential to enjoy all its benefits.
Conclusion
Efficient healthcare revenue cycle management is not merely a sequence of steps but a holistic, strategic approach that combines technology, data-driven insights, compliance, and patient engagement. Using automated tools and software, can significantly streamline administrative procedures and enhance the patient experience.
This approach reduces costs and increases revenue, contributing to the overall growth and success of the medical practice. At the heart of this process is the patient, whose experience can be significantly improved through clear communication, accurate billing, and a smooth, efficient process.
The path to successful healthcare RCM doesn’t have to be complex. With BellMedex, you can navigate the intricacies of this process with ease. BellMedex offers robust RCM solutions tailored to your needs, helping you enhance efficiency, maintain compliance, and improve patient satisfaction.
Embrace the future of healthcare revenue cycle management with BellMedex, and witness the transformation in your practice’s revenue and patient experience. Your journey to a better, more efficient revenue cycle begins here. Contact BellMedex today.