Are you in hot water because you submit documents and insurance claims without adding formal transfer of care. Don’t worry!
The Office of Inspector General (OIG) has updated its 2025 Work Plan and is focusing on reviewing postoperative services that are part of the global surgery period. With the recent changes in the global surgery coding system for 2025, it’s essential for healthcare professionals to stay up-to-date.
The OIG (Office of Inspector General) is examining how these postoperative services are being provided and billed during the global surgery period. This could involve checking for compliance, accuracy in billing, or identifying issues like overbilling or lack of quality of care.
For healthcare providers, it is important to understand the 2025 global surgery updates as it could impact their practices of documenting the surgery procedures and billing for services. However, for patients it is also vital as it lets them receive proper care during the recovery period and improve transparency.
This guide will help you walk through the new coding requirements, postoperative services, and how to comply with Medicare regulations. But, first let’s discuss the global surgical period.
What Is a Global Surgery Package?
A Global Surgery Package, also known as global surgery or the global period is a Medicare concept where payment for a surgical procedure includes the surgery itself and related services provided before, during, and after the surgical procedure. These services are bundled into a single payment, covering preoperative visits, the surgical procedure, and postoperative care (follow-up visits) within a specified time frame usually ranging from the day of surgery to 10 or 90 days after the surgery.
If providers in the same group and specialty are involved in the surgical procedure, they must submit their bills and accept payment as if they’re one provider. This keeps billing simple and avoids double charges.
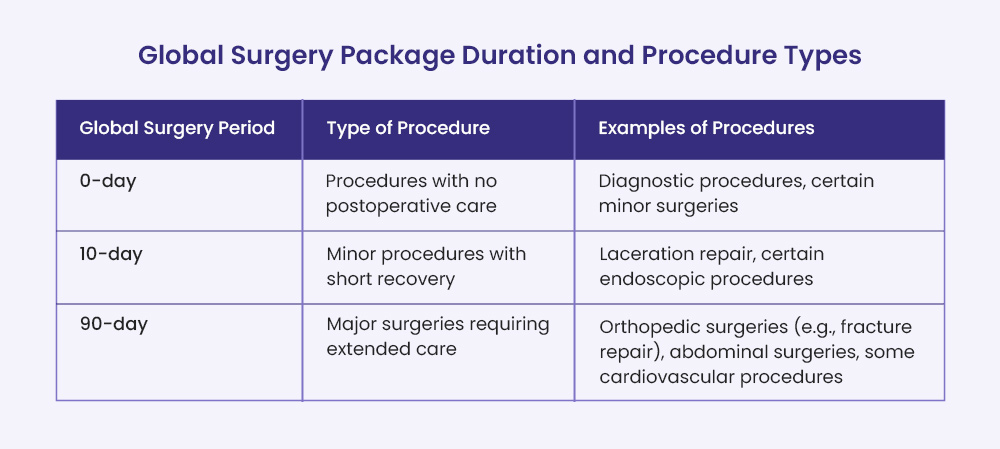
Global Surgery Package Duration and Procedure Types
| Global Surgery Period | Type of Procedure | Examples of Procedures |
| 0-day | Procedures with no postoperative care | Diagnostic procedures, certain minor surgeries |
| 10-day | Minor procedures with short recovery | Laceration repair, certain endoscopic procedures |
| 90-day | Major surgeries requiring extended care | Orthopedic surgeries (e.g., fracture repair), abdominal surgeries, some cardiovascular procedures |
CMS Guidelines for Global Surgery Period—What Is Included in The Global Surgery Package?
For Medicare claims, CMS (Centers for Medicare & Medicaid Services) includes the following services in the global surgery payment:
- Preoperative Visits
- Intraoperative Services
- Other Medical or Surgical Services in the Postoperative Period
- Postoperative Follow-Up Visits
- Post-Surgical Pain Management
- Supplies
- Miscellaneous Services

Preoperative Visits
These are visits that happen after the decision to operate has been made during the evaluation and management process (E/M). This includes minor surgeries or endoscopy procedures performed by the same provider on the same day as the surgery.
Intraoperative Services
These are services provided during the actual surgery, including everything necessary to perform the surgical procedure.
Other Medical or Surgical Services in the Postoperative Period
All other medical or surgical services after the surgical procedure include any additional medical or surgical care that the surgeon provides to the patient during the designated recovery time after the surgery.
Postoperative Follow-Up Visits
These are check-ups or follow-up appointments to monitor the patient’s recovery during the postoperative period. Usually the code 99024 is used to track the follow-up visits.
Post-Surgical Pain Management
Post-Surgical Pain Management includes care provided to help the patient manage pain after the surgery, such as medication or therapy.
Supplies
These are materials used during the surgery and recovery period, except for certain excluded items. For example, bandages or surgical tools.
Miscellaneous Services
These are smaller, routine tasks related to surgery, such as bandage changing, local incision care, operative pack removal, cutaneous sutures and staples removal, etc.
CMS guidelines for global surgery Period— What Isn’t Included in the Global Surgical Package?
Here are certain services that CMS does not include in the global surgical package, and what providers can bill separately and get paid.
- Initial Evaluation for Surgery
- Services by Other Providers
- Unrelated Visits
- Treatment for Separate Health Conditions
- Diagnostic Tests
- Additional Surgeries
- Complication Treatment in OR (Operating Room)
- Failed Minor Procedure Leading to Major Surgery
- Organ Transplant Medications
- Critical Care Services

Initial Evaluation for Surgery
The surgeon’s decision on the first visit to evaluate if major surgery is needed is not part of the global surgical package. The evaluation visit (E/M) can be billed separately using modifier 57.
Services by Other Providers
If other providers (not the surgeon) perform surgery-related services, these are excluded from the package unless there’s an agreement to transfer care between the surgeon and other providers. This agreement must be documented in the patient’s medical records.
Unrelated Visits
Follow-up visits for conditions unrelated to the surgery or its diagnosis are not included in the global surgery package, except when visits are due to surgery complications.
Treatment for Separate Health Conditions
If a patient needs treatment for an underlying or unrelated health condition, or begins a new treatment unrelated to surgery recovery, it’s billed separately.
Diagnostic Tests
Tests or procedures to diagnose issues (like X-rays or other scans) are not included in the package and require separate billing.
Additional Surgeries
Surgeries performed during the recovery period that are not part of the original surgery or related to surgery complications are excluded from the Medicare global surgery package.
Complication Treatment in OR (Operating Room)
If the patient needs to return to the OR for postoperative complications, the treatment is billed separately.
Failed Minor Procedure Leading to Major Surgery
When a less serious surgery doesn’t work and a major surgery is needed, Medicare covers the major surgery separately.
Organ Transplant Medications
Medications used to manage the immune system after an organ transplant are not part of the global surgical package.
Critical Care Services
Critical care provided (CPT codes 99291 and 99292) after surgery for issues unrelated to the surgical procedure is excluded. These services should be billed separately using modifier FT.
2025 Global Surgery Updates
The 2025 global surgery package updates bring key changes, including the introduction of HCPCS code G0559, which is used for postoperative follow-up visits provided by a different healthcare professional who didn’t perform the surgery, within the 90-day global period, and without a formal transfer of care.
Modifiers 54, 55, and 56 are now more strictly required for managing preoperative, surgical, and postoperative care within 90-day global packages, with modifier 56 now requiring formal documentation for preoperative care transfers.
The updates also focus on the Office of Inspector General’s (OIG) review of postoperative services, ensuring proper reporting and preventing overreporting of services during the global period. These updates aim to improve billing practices and ensure accurate Medicare reimbursement for global surgeries.
The Role of the OIG and CMS in Global Surgery Coding 2025
The Office of Inspector General (OIG) is investigating how well postoperative services are reported under Medicare’s global surgery payment system. Since July 1, 2017, Medicare requires healthcare providers to report follow-up visits after surgery using a specific code, CPT code 99024. This code is for postoperative visits where the doctor checks the patient’s recovery after surgery. Although these visits are part of the global period and aren’t paid separately during the global period, reporting them helps Medicare track how often patients need follow-ups after surgery.
Here is when providers have to report postoperative visits using code 99024 under specific conditions: ⬇️
- Practitioners in certain states (like Florida, Kentucky, Louisiana, Nevada, New Jersey, North Dakota, Ohio, Oregon, Rhode Island) who work in groups with 10 or more practitioners.
- Providers in those states need to check a list from Medicare each year to see if their surgeries are on the list of surgeries that need the code.
- This code applies only to specific types of surgeries or procedures. These procedures are selected by Medicare because they are either very common (performed over 10,000 times a year) or very expensive (with charges over $10 million a year).
The OIG (Office of Inspector General) is monitoring that doctors are reporting these follow-up visits correctly. They will look at a sample of global surgeries, compare the number of follow-up visits in the CMS records with what doctors reported to Medicare, and verify if the payments made for the surgeries match the actual care provided to Medicare beneficiaries. If doctors don’t report this information properly, it could lead to Medicare paying less for those surgeries. If providers don’t report this information properly, it could lead to devaluation of the Medicare global surgery payment.
Basically, Medicare wants to check the follow-up visits after surgery are being properly tracked, and if doctors aren’t reporting them correctly, it might affect their payment.
Importance of Using Modifiers During Global Surgery Period
Sometimes, a patient may need other procedures that aren’t related to the surgery they just had, but these procedures still happen during the global period. The usage of global surgery modifiers (24, 25, 54, 55, 57, 58, 78, 79, FT) facilitate healthcare providers to get paid for these services. These modifiers are used to separate unrelated procedures from the global surgery, so they can be paid for separately, even if they happen during the global period.
In the Medicare Physician Fee Schedule (MPFS), there are certain payment policy indicators that show which services are billable (can be paid for) and whether a modifier is needed.
Some examples of global modifiers include:
- Modifier 24: Used for services unrelated to the surgery but happening during the global period.
- Modifier 25: Used for an unrelated service provided on the same day as the surgery.
- Modifiers 54, 55, 57, 58, 78, 79: Indicate different situations where services are not included in the global period.
- Modifier FT: Used for specific cases defined by Medicare.
| Modifier | Description | When to Use | Key Points |
| 24 | Unrelated evaluation and management (E/M) service | During the postoperative period for unrelated care | Applies when care is for an issue not related to the original surgery. |
| 25 | Significant, separately identifiable E/M service | On the same day as a procedure | Used when an additional E/M service is required apart from the surgical procedure. |
| 57 | Decision for surgery | When an E/M service leads to the decision for surgery | Applied to indicate that the surgery was decided during the E/M visit. |
| 54 | Surgical care only | When only the surgery is provided | The surgeon is not responsible for pre-operative or postop care. |
| 55 | Postoperative care only | When another provider manages postoperative care | Used after a formal transfer of care from the surgeon. |
| 56 | Preoperative care only | When another provider manages pre-operative care | Indicates pre-op care without involvement in the surgery or postop care. |
| 58 | Planned or staged procedure | For planned or related follow-up procedures | Use for treatments planned as part of the surgical procedure. |
| 78 | Unplanned return to the operating room | For related complications requiring further surgery after the original surgery | Indicates an unexpected return to address a complication. |
| 79 | Unrelated procedure or service | For a new, unrelated surgery during global period | Used when the procedure is unrelated to the initial surgery. |
| FT | Unrelated E/M service during global period | For unrelated E/M service on the same day | Used for E/M services distinct from the surgery. |
➜ Modifiers 24
Modifier 24 is used when a doctor or healthcare provider performs unrelated evaluation and management (E/M) service. These services must be after the procedure but within the global period and are unrelated to the original surgical procedure.
For example:
On March 10, a patient visits their orthopedic surgeon for a knee arthroscopy (CPT 29881), which has a 90-day global period. On March 15, the patient returns to the same surgeon, complaining of new back pain unrelated to the knee surgery. The surgeon evaluates the patient’s back condition and recommends physical therapy for the back pain. Since this visit is not related to the knee arthroscopy, the surgeon will code the appropriate office visit E/M code with modifier 24. This allows the surgeon to be separately paid for the back-pain evaluation, even though it falls within the global period for the knee surgery.
➜ Modifier 25
This modifier is used when the same physician or other qualified healthcare professional performs a significant, separately identifiable evaluation and management (E/M) service on the same day as a procedure or other service.
For example:
A patient arrives at the doctor’s office on the same day they are scheduled for gallbladder removal surgery (CPT 47562 – Laparoscopic Cholecystectomy). During the pre-surgery evaluation, the doctor notices that the patient has significantly high blood pressure. The doctor spends extra time assessing the patient’s blood pressure, determining the cause, and prescribing immediate medication to stabilize the patient before proceeding with surgery.
In this case, the additional evaluation and management (E/M) service for high blood pressure is beyond the usual preoperative care related to the gallbladder surgery. The doctor can use Modifier 25 to bill separately for the extra E/M service.
➜ Modifier 57
Use of Modifier 57 indicates that a decision for surgery was made during an evaluation and management (E/M) service, and that the decision occurred on the same day as the E/M service. This modifier tells the payer that the E/M visit led to a decision for surgery, and because the decision was made during the same visit, the surgery is being reported separately from the usual preoperative care.
For example:
A patient arrives at the emergency room (ER) after experiencing severe abdominal pain. The ER physician performs an evaluation and determines that the patient may have acute appendicitis. After a thorough examination and some tests, the physician discusses the situation with the patient and recommends immediate surgery to remove the appendix.
The decision for surgery is made during the evaluation and management (E/M) service in the ER. The patient is then taken to the OR on the same day for an appendectomy (removal of the appendix).
Since the decision for surgery was made during the E/M service on the same day, the ER physician uses Modifier 57 when reporting the E/M code. This modifier indicates that the E/M visit led directly to the decision for surgery, which occurred on the same day.
➜ Modifier FT
Using Modifier FT indicates an unrelated evaluation and management (E/M) visit during a postoperative period or on the same day as a procedure or another E/M visit. The key aspect here is that the E/M service is unrelated to the procedure that was performed or is planned, and it may be billed separately. This modifier applies when an E/M service is provided that is unrelated to the surgery or procedure performed on the same day or within the global surgical period. It is particularly relevant when a patient requires critical care during the postoperative period, which is unrelated to the surgery.
For example:
A patient undergoes gallbladder surgery (CPT® 47562) on March 10. On the same day, the patient develops a severe allergic reaction unrelated to the surgery, requiring urgent treatment and evaluation. The physician uses Modifier FT to report the E/M service provided on March 10 for the allergic reaction as unrelated to the gallbladder surgery. This ensures the physician gets reimbursed for both the surgery and the unrelated E/M service provided on the same day.
Procedural Modifiers 54, 55, 56
Modifiers 54, 55, and 56 are used to split reimbursement between two different healthcare providers when the surgical procedure and preoperative/postoperative care are managed by separate physicians. This is often referred to as a “transfer of care” and helps ensure that both the surgeon and the other providers (such as a primary care physician) are appropriately reimbursed for their role in the patient’s care.
- Modifier 54 (Surgical Care Only)
Modifier 54 is used by the surgeon who performs the surgery but does not provide preoperative or postoperative care.
- Modifier 55 (Post-Operative Management Only)
Modifier 55 is used by the physician or provider who takes over post-operative care after the surgery is completed. It applies when the provider does not perform the surgery but manages the recovery phase instead. After a surgery is performed in one hospital, the patient may be transferred to a different location, and a different physician will provide follow-up care for the post-operative recovery period.
- Modifier 56 (Pre-Operative Management Only)
This modifier is used when the physician or provider who manages the preoperative care of the patient. It applies when the provider does not perform the surgery but is responsible for preparing the patient before the surgery, such as clearing them for anesthesia or managing their health conditions. For example, a primary care provider may ensure the patient is ready for surgery, while a different physician performs the procedure.
These modifiers are used when two different healthcare providers (such as a surgeon and a hospitalist or a primary care physician) are involved in a patient’s surgical care, especially when the care is split between preoperative, surgical, and postoperative periods.
According to 2025 global surgery updates, CMS will require these modifiers for all 10 to 90-day global surgical packages, ensuring accurate reimbursement for each phase of surgical procedure.
For example:
A patient comes to the ER with a dislocated shoulder. The ED physician performs a closed reduction and reports the procedure with Modifier 54 for surgical care only. The patient is then referred to an orthopedic specialist for postoperative care, and the orthopedic doctor reports the same procedure code with Modifier 55. If the patient had seen a primary care provider (PCP) before the surgery for preoperative management, the PCP would have reported their care with Modifier 56 for preoperative care only. All providers use the same date for the procedure on their claims.
➜ Modifier 58
Adding modifier 58 indicates that a staged or related procedure was performed by the same physician (or other qualified healthcare professional) during the post-operative period of a previous procedure. This modifier specifies that the new procedure or service is planned, expected, or necessary due to the patient’s condition and is related to the initial surgery. Modifier 58 resets the global period, starting a new one for the next procedure.
For example:
A patient undergoes a knee replacement surgery. As part of the surgical plan, the surgeon schedules a follow-up arthroscopic procedure to inspect and adjust the placement of the knee prosthesis after the initial healing phase. This follow-up procedure is planned in advance and is related to the initial surgery. When the patient returns during the global period of the knee replacement for the planned arthroscopic procedure, the surgeon reports the follow-up procedure with Modifier 58 to indicate that it is a staged and related procedure.
➜ Modifier 78
Modifier 78 is used for an unplanned return to the operating room when a patient requires a related procedure during the postoperative period due to complications from the initial surgery, such as infection or bleeding. This modifier indicates that the same physician, or a healthcare professional from the same specialty group, performs the second procedure to address the issue. The second procedure is considered part of the original surgery and does not start a new global period. For repeat procedures, Modifier 76 should be used.
For example:
During the global period of a surgery, the patient experiences excessive bleeding, requiring the surgeon to return to the operating room to control it. This procedure is reported with Modifier 78 to indicate it is an unplanned related procedure performed during the postoperative period.
➜ Modifier 79
Modifier 79 is used when a physician performs an unrelated procedure or service during the postoperative period of a prior surgery. This procedure is not related to the initial surgery and must be billed separately, as it is not covered by the original surgery’s global package. If a procedure is repeated on the same day, Modifier 76 should be used.
For example:
On March 5, a patient undergoes knee replacement surgery on the right leg. On April 5, the patient undergoes the same surgery on the left leg. Even though it’s the same procedure for the same diagnosis, the surgeries are performed on two different surgical sites, making them unrelated. Modifier 79 is appended to the medical code for the surgery on April 5 to indicate it is a separate, unrelated procedure performed during the postoperative period of the first surgery.
Best Practices for Global Surgery Coding Compliance

By following these best practices, healthcare providers can stay compliant with global surgery coding requirements:
Use Proper Documentation
- Keep complete and accurate documentation for all care services provided before, during, and after the surgical procedure.
- Maintain clear records for transfer of care, especially when other providers are involved in preoperative, surgical, or postoperative care.
Know the Global Surgery Period
- Understand the global surgery period for each surgical procedure and apply it correctly. For example, some procedures may have a 10-day, 90-day, or 0-day global period as explained in the table above.
- Review the global surgery indicators assigned to each procedure (e.g., 000, 010, 090) to confirm the global period for billing purposes.
Use Proper Modifiers
- Use the correct modifiers when services are provided that are outside the scope of the global surgery package.
Properly Apply HCPCS Code G0559
- According to the 2025 global surgery period, use HCPCS code G0559 for post-operative follow-up visits by a healthcare provider who did not perform the surgery, and there was no formal transfer of care.
Review Medicare Physician Fee Schedule (MPFS)
- Check the MPFS for global surgery package indicators (e.g., 000, 010, 090) and understand the rules for each CPT code.
Comply with OIG Guidelines
- Adhere to Office of Inspector General (OIG) requirements for reporting postoperative services, especially for evaluation and management (E/M) services.
- Use CPT code 99024 for postoperative E/M visits where required, particularly in states that require reporting for global surgeries.
Accurate Reporting of Postoperative Care
- Report only care services that are directly related to the original surgical procedure. Do not report services outside of the global package unless they are unrelated or involve complications.
- If a procedure or service is unrelated to the original surgery, apply the correct modifier (e.g., modifier 79).
Provide Transfer of Care Documentation
- Document formal transfers of care when the patient’s care is transferred between providers, especially for preoperative and postoperative care.
- Use modifier 56 for preoperative services and modifier 55 for postoperative services when the care is performed by different providers.
Stay Updated on CMS and OIG Changes
- Regularly review updates from CMS and the OIG to stay compliant with new coding guidelines or updates as they released global surgery period 2025 updates, such as the use of HCPCS code G0559 for postoperative follow-up visits.
FAQs
Does global surgery payment only apply to inpatient hospital settings?
Global surgery applies to all settings, such as hospitals (inpatient and outpatient), ambulatory surgical centers (ASCs), and doctors’ offices. Surgeon visits to Medicare patients in intensive or critical care units are also included in the global surgical package.
How does Medicare define the global surgical package?
Medicare classifies 3 types of global surgical packages based on the number of post-operative days.
a). 0-Day Post-Operative Period (Endoscopies and Minor Procedures):
No pre-operative period.
No post-operative period.
Visits on the procedure day are not billed separately.
b). 10-Day Post-Operative Period (Other Minor Procedures):
No pre-operative period.
Visits on the procedure day are not billed separately.
Covers 11 days: the surgery day and 10 days after.
c). 90-Day Post-Operative Period (Major Procedures):
Includes 1 day of pre-operative care.
Visits on the procedure day are not billed separately.
Covers 92 days: 1 day before surgery, the surgery day, and 90 days after.
What is the difference between modifier 24 and modifier 79?
Modifier 24 and Modifier 79 are both used to report services during the postoperative period, but they are used in different situations:
Modifier 24 – Unrelated E/M service during the postoperative period.
Modifier 79 – Unrelated procedure during the postoperative period.
What is the difference between modifier 24 and modifier FT?
Modifier 24 is used for unrelated E/M services provided during the postoperative period, but not on the same day as a procedure or surgery.
Modifier FT is used for unrelated E/M services provided on the same day as a procedure or another E/M service during the global period, such as critical care or another medically necessary service that is unrelated to the surgery.
What is “Transfer of Care”?
In the global surgery period, “Transfer of Care” refers to the formal handover of responsibility for a patient’s post-operative care from the surgeon or surgical team to another healthcare provider who is not part of the surgical team. The process involves clear communication and sharing of the patient’s surgical details, medical records, and care plans. Transfer of care is crucial in situations where the original surgeon is unavailable or specialized post-operative care is required.
What is HCPCS code G0559 used for?
HCPCS code G0559 refers to a post-operative follow-up visit that involves evaluation and management services addressing surgical procedures. This code is used when the follow-up care is provided by a physician or qualified healthcare professional who is not the practitioner who performed the surgery (or is not in the same group practice). It applies within the 90-day global period of the procedure and includes tasks like reviewing surgical notes, researching the procedure, examining the patient, and communicating with the original practitioner if needed.
Can post-operative care be billed separately during the global period?
No, post-operative care related to the surgery is generally included in the global surgical package and cannot be billed separately. However, exceptions apply, such as using HCPCS code G0559 for follow-up care provided by a different physician not in the same practice as the surgeon.
How does HCPCS code G0559 differ from CPT code 99024?
HCPCS code G0559 is used for post-operative follow-up care provided by a different physician, outside of the original surgeon’s practice, during the global period. CPT code 99024, on the other hand, is used for tracking post-operative visits provided by the same surgeon or their group and is not reimbursable.
Why would Medicare pay separately under HCPCS code G0559 if post-operative care is already included in the global surgical package?
While post-operative care is bundled into the global surgical package, Medicare recognizes there are situations where it is tough for the original surgeon to provide follow-up care. These include cases where the patient relocates, specialized expertise is required, or the original surgeon is unavailable. In such scenarios, HCPCS code G0559 allows a different physician to provide necessary post-operative care and be reimbursed separately, facilitating the patient to receive timely and appropriate follow-up care.
Is there a limit to the number of follow-up visits a different physician can bill under HCPCS code G0559?
There is no specific limit to the number of follow-up visits that can be billed under HCPCS code G0559. However, each visit must be justified as medically necessary and directly related to the surgical procedure. The documentation should include details of each visit, such as the patient’s condition, evaluation findings, and any interventions. Excessive or unjustified billing may be flagged during audits, so accurate and thorough records are critical.
How does Medicare verify that follow-up care billed under G0559 is related to the original surgery?
Medicare requires comprehensive documentation to verify that follow-up care billed under G0559 is related to the original surgery. This includes references to the surgical procedure, diagnosis codes that align with the reason for post-operative care, and a detailed account of the services provided. Medicare may also review the patient’s surgical records and related documentation during audits to confirm that the follow-up care is consistent with the standard of care for the procedure.
Are there penalties for improperly using G0559 or modifiers 54, 55, and 56?
Yes, improper use of G0559 or modifiers 54, 55, and 56 can result in claim denials, financial penalties, and potential audits. If Medicare determines that these codes or modifiers were used incorrectly or fraudulently, the provider may have to repay the amount reimbursed and could face additional fines or legal actions.
Can modifiers 54 and 55 be used when the providers are from entirely different practices?
No, modifiers 54 and 55 are used when providers are in the same group practice but split the global package responsibilities and reimbursement.
How do private insurers handle situations similar to HCPCS code G0559?
Private insurers often have their own policies and guidelines, which may align with Medicare’s rules or differ based on their payment structure. In many cases, private insurers require similar coding and documentation to justify post-operative care provided by a different physician. It’s important to review the specific insurer’s policies to understand how they handle these cases and whether they recognize codes like G0559 for separate reimbursement.