Key Insights
➟ In 2024, Medicare will increase daily rates for Skilled Nursing Facilities (SNFs) by 4%. This will add $1.4 billion in spending.
➟ Medicare Part A pays for up to 100 days of skilled nursing care, but patients must meet certain requirements.
➟ The cost of skilled nursing care is different in each state. For example, in Texas, the average daily rate is about $180, while in New York City, it can be more than $422 for semiprivate rooms.
➟ After the first 20 days of Medicare coverage for skilled nursing care, patients must pay a daily fee of about $204 for days 21 to 100.
How could the new CMS rules change things for your SNF?
As the sun rises and sets, so does the journey through health’s trials.
I mean, as we age, we really do face healthcare challenges along the way.
And when intense care is needed, a skilled nursing facility (SNF) is usually the best choice. However, you have options — a short stay to recover or a permanent move from the SNF to a nursing home.
Therefore, knowing the daily rates for each guides smart decisions.
Medicare pays SNFs different daily rates compared to nursing homes. Rates change every year, with important updates in 2024. The Centers for Medicare & Medicaid Services (CMS) say there will be a 4% increase in daily rates for skilled nursing facilities (SNF) in 2024. This means about $1.4 billion more will be spent. 🔗
These SNF costs are projected to climb up to 4.1% in 2025, thus raising the possibility of further price escalations.
So it is important for SNF staff to know about rate changes to bill correctly.
🧐 Does knowing about the Medicare Daily Rate even matter to me as a patient?
If you are a patient, then staying informed about Medicare’s daily rates for skilled nursing facilities is important as well.
The daily rates for SNF change depending on the state, region, and provider. Costs vary depending on how long you stay, whether you choose a private or semi-private room, and the services you use. When you look at SNF options, understanding the rates will help you make choices that fit your care needs and budget.
Taking action now, when care needs are not as strong, helps you get good and affordable care later.
Skilled Nursing Care Rates By Location
The price of skilled nursing care can change a lot based on where you are. This difference in rates allows Medicare beneficiaries to move to another area or state to find more affordable care while living in a nursing facility or nursing home. Picking a place with cheaper prices can help seniors make their benefits last longer.
Skilled Nursing Facility Rates By State
The costs of skilled nursing facilities change based on where they are located. So, some states have SNFs that charge a lot, while other states have SNFs that charge less. The table below shows the average monthly costs of nursing homes.
| State | Median Monthly Cost (Semiprivate Room) | Median Monthly Cost (Private Room) |
| Alabama | $7,832 | $8,302 |
| Alaska | $19,267 | $35,622 |
| Arizona | $7,832 | $9,712 |
| Arkansas | $7,206 | $8,145 |
| California | $11,748 | $13,628 |
| Colorado | $9,759 | $10,746 |
| Connecticut | $15,508 | $17,074 |
| Delaware | $11,467 | $12,250 |
| District of Columbia | $13,002 | $14,099 |
| Florida | $10,182 | $11,748 |
| Georgia | $8,177 | $8,616 |
| Hawaii | $12,532 | $12,563 |
| Idaho | $10,809 | $11,404 |
| Illinois | $7,676 | $8,929 |
| Indiana | $8,114 | $9,994 |
| Iowa | $8,616 | $9,242 |
| Kansas | $7,707 | $8,240 |
| Kentucky | $8,004 | $9,179 |
| Louisiana | $7,112 | $7,707 |
| Maine | $12,563 | $13,550 |
| Maryland | $11,858 | $13,221 |
| Massachusetts | $14,099 | $15,038 |
| Michigan | $10,887 | $11,811 |
| Minnesota | $10,589 | $13,189 |
| Mississippi | $8,773 | $9,023 |
| Missouri | $6,109 | $6,736 |
| Montana | $8,427 | $8,710 |
| Nebraska | $7,832 | $8,334 |
| Nevada | $10,511 | $12,767 |
| New Hampshire | $12,344 | $13,315 |
| New Jersey | $11,968 | $13,080 |
| New Mexico | $9,023 | $10,307 |
| New York | $14,395 | $15,257 |
| North Carolina | $8,616 | $9,399 |
| North Dakota | $8,145 | $8,851 |
| Ohio | $8,616 | $9,806 |
| Oklahoma | $6,109 | $7,049 |
| Oregon | $15,023 | $15,664 |
| Pennsylvania | $11,091 | $11,095 |
| Rhode Island | $12,532 | $13,941 |
| South Carolina | $8,929 | $9,649 |
| South Dakota | $8,835 | $9,179 |
| Tennessee | $8,914 | $9,555 |
| Texas | $5,483 | $6,893 |
| Utah | $7,832 | $10,417 |
| Vermont | $13,628 | $14,568 |
| Virginia | $9,524 | $10,496 |
| Washington | $12,532 | $14,099 |
| West Virginia | $11,968 | $12,313 |
| Wisconsin | $10,558 | $10,496 |
| Wyoming | $7,832 | $9,712 |
What Are The States With The Most Affordable Nursing Home Care?
Here is a list of top 10 states with the most affordable nursing home care.
| State | Median Daily Cost (Semiprivate Room) | Median Daily Cost (Private Room) |
| Texas | $180 | $227 |
| Missouri | $201 | $221 |
| Oklahoma | $201 | $232 |
| Louisiana | $234 | $253 |
| Arkansas | $237 | $268 |
| Illinois | $252 | $294 |
| Kansas | $253 | $271 |
| Alabama | $258 | $273 |
| Nebraska | $258 | $274 |
| Georgia | $269 | $283 |
Nursing Home Costs in the U.S. Cities
| City | Median Daily Cost (Semiprivate Room) | Median Daily Cost (Private Room) |
| New York City, NY | $422 | $458 |
| Los Angeles, CA | $361 | $449 |
| Chicago, IL | $2294 | $402 |
| Houston, TX | $194 | $258 |
| Phoenix, AZ | $271 | $337 |
| Philadelphia, PA | $455 | $484 |
| San Antonio, TX | $180 | $216 |
| San Diego, CA | $391 | $515 |
| Dallas, TX | $193 | $243 |
| Austin, TX | $218 | $267 |
💢 Fed up with manual claims processing at your SNF?
Are you wasting too much time entering claims data by hand? Use our automation technology now to simplify your SNF’s billing, cut errors, and boost your revenue cycle.
How Can You Differentiate Between A Skilled Nursing Facility And A Nursing Home?
“Skilled nursing facility” and “nursing home” are words that people often use the same way, but they actually mean different types of care places with important differences. The main differences are in how long you stay, the care you get, the services available, and how you pay.
Duration of Stay:
Skilled Nursing Facilities (SNFs) are meant for short visits. They help people who are recovering from all illness, injury, or surgery. These facilities give short-term medical help and rehabilitation services. They assist patients in getting back their independence so they can go home or move to a long-term care facility if necessary.
In contrast, Nursing Homes are places for long-term care. They help people who need support with daily activities because of long-term health issues or aging problems.
Level of Care:
SNFs provide more medical care and supervision than nursing homes. They have trained healthcare workers, like registered nurses, practical nurses, physical therapists, occupational therapists, and speech therapists. These experts work as a team to give complete medical care, rehabilitation help, and skilled nursing services that are designed for each patient’s unique needs.
Nursing homes, on the other hand, mainly offer basic medical care and help with daily activities like bathing, dressing, eating, and moving around. Nursing homes usually have licensed nurses, but they do not have as many different types of medical specialists as skilled nursing facilities (SNFs).
Services Provided:
Along with skilled nursing care, SNFs provide various services to help patients recover and rehabilitate. These services can include care after surgery, taking care of wounds, managing pain, giving medicine through IV, physical therapy, help with daily activities, and speech therapy. SNFs also offer 24-hour emergency services and special equipment to help with recovery.
Nursing homes, in contrast, provide long-term care for people who need help with daily activities, taking medicine, and basic health care. They might provide fun activities, help for social needs, and transportation services to improve the lives of residents.
Payment Methods:
Medicare usually pays for SNFs for a short time if the patient meets specific requirements, like being admitted from a hospital within a certain period. Nursing home care, on the other hand, is often paid for through a combination of private funds, long-term care insurance, and Medicaid (for those who qualify based on income and asset levels).
Some places may provide both skilled nursing and long-term care services, making it hard to tell the difference between SNFs and nursing homes. However, understanding the differences between these two types of care facilities can help people and their families choose the best care option for their needs and situations.
Medicare Coverage For Skilled Nursing Care Facilities
Medicare coverage for skilled nursing care facilities is based on two main things: where the facility is located and how long you stay there. Additionally, patients need to follow specific rules from Medicare to qualify for coverage.
For example, Medicare Part A pays for up to 100 days of care in a shared room during each benefit period. This is for when a skilled nursing facility meets Medicare’s requirements. A benefit period starts when you enter a hospital or skilled nursing facility and ends when you have been out of the facility for 60 days in a row.
To qualify, you must have a qualifying hospital stay of at least 3 days before going to the skilled nursing facility. You must also need daily skilled care like intravenous medications or physical therapy. In addition, a doctor must confirm that you need skilled care within 30 days after you are admitted. You can get coverage for a maximum of 100 days each time you use your benefit period.
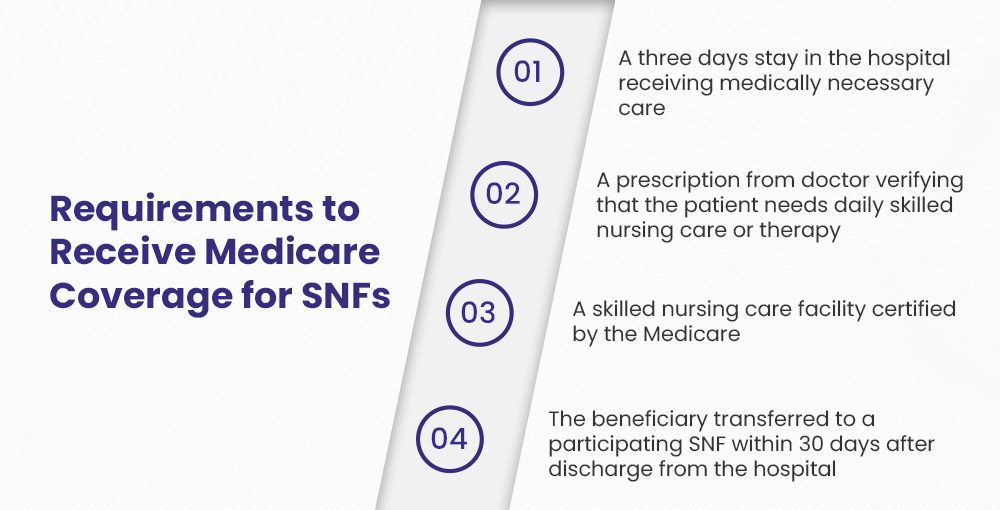
Requirements for Medicare Coverage of Skilled Nursing Facilities
1️⃣ The patient needs to stay in the hospital for at least three days to get important medical care. This stay is for situations that need skilled nursing care afterwards.
2️⃣ A doctor must give a prescription that shows the patient needs daily skilled nursing care or therapy. This care should be done by, or with help from, qualified professionals or technical staff, making sure that the services follow Medicare standards.
3️⃣ The skilled nursing facility (SNF) needs to be approved by Medicare. This certification shows that the facility follows important health and safety rules set by the government.
4️⃣ The patient must be transferred to a participating skilled nursing facility within 30 days of being discharged from the hospital. This requirement is crucial for maintaining eligibility for coverage.
5️⃣ The patient must be enrolled in Medicare Part A, which covers inpatient hospital stays and certain skilled nursing facility services.
6️⃣ The services provided in the skilled nursing facility must be deemed medically necessary and appropriate for the patient’s condition, as determined by their healthcare provider.
7️⃣ Patients might need to have regular assessments to make sure they still qualify for skilled nursing services. This includes progress evaluations by healthcare professionals.
8️⃣ Medicare usually pays for skilled nursing care for up to 100 days in each benefit period. The first 20 days are fully covered, but for the next 80 days, there is a copayment required. In 2024, the coinsurance is about $204 each day.
9️⃣ The patient needs skilled nursing care every day. This care can include things like taking care of wounds, giving medicine through an IV, or helping with rehabilitation.
🔟 The need for skilled nursing must be clearly justified based on the patient’s medical condition and treatment plan, ensuring that the care provided aligns with their health needs.
Out-of-Pocket Costs for each Benefit Period:
- Days 1-20: Patients pay $0.
- Days 21-100: Patients are responsible for coinsurance of up to $204 per day.
- Days 101 and beyond: Patients cover all costs.
Reminder: Medicare does not pay for some things, like TVs, phones, private room fees (unless medically necessary), or private nursing services. For example, if your doctor recommends services that are not covered by Medicare, you will not be compensated for them.
⚔️ Facing Medical Billing Denials at Your Skilled Nursing Facility?
Is your SNF struggling with a high denial rate that’s hurting profits? Our team can quickly help you find and fix denial reasons, improve your coding, and boost your reimbursement rates.
What is a Benefit Period in Skilled Nursing Facility?
A benefit period refers to the way Medicare measures your use of hospital and skilled nursing facility (SNF) services. It determines how much coverage you will receive from Medicare Part A for inpatient care.
Each benefit period begins the day you are admitted as an inpatient to a hospital or SNF. The benefit period ends when you have not received inpatient care in either a hospital or SNF for 60 consecutive days. At that point, if you need to be admitted again, a new benefit period will begin.
During each benefit period, Medicare Part A provides coverage for your inpatient care according to certain limits:
- For hospital care, Medicare Part A covers up to 90 days. You pay a deductible for days 1-60 and a coinsurance amount for days 61-90.
- For SNF care, Medicare Part A covers up to 100 days. You pay nothing for the first 20 days. For days 21-100, you pay a daily coinsurance amount.
For example, let’s say you are admitted to the hospital for 5 days due to pneumonia. This starts your benefit period. Two months later, you fall and break your hip, requiring another hospital stay of 4 days. This is still the same benefit period because less than 60 days passed between your hospital stays.
After your hip heals, you transfer to a SNF for rehabilitation for 30 days. Those SNF days also apply to the same benefit period. In total for this benefit period so far, you have used 9 hospital days and 30 SNF days. If you need more inpatient care, your coverage will depend on how many benefit days you have left.
Skilled Nursing Care Billing Tips
Skilled nursing facilities can use these important billing tips to help prepare and submit claims for Medicare beneficiaries accurately and correctly:
Understand Utilization Days: It is important to know that the last day of care—this could be the day you leave the hospital, the day of death, or the first day of a leave of absence (LOA)—is not counted as a utilization day for billing. This means facilities should not charge for these days.
Discharge Policy: If a patient covered by Medicare leaves but comes back before midnight on the same day, Medicare does not count this as a discharge. So, billing should reflect the patient’s continuous stay, because it impacts the total days used.
Accurate HIPPS Rate Coding: Make sure that the HIPPS rate code matches exactly with the assessment that was submitted and accepted by the state where the skilled nursing facility is located. Any mistakes can cause claims to be denied or payments to be delayed.
Clear Documentation: Keep clear and correct records of all services given. This includes daily notes, care plans, and any changes in a patient’s condition. Good documentation helps show why services billed to Medicare are needed.
Ongoing Training for Staff: Provide regular training for your billing staff to ensure they know the latest Medicare rules, coding updates, and compliance needs. This active method can greatly lower mistakes and improve the accuracy of claim submissions.
Claim Submission: Submit claims on time to prevent delays in getting your money back. Learn the specific deadlines for submitting documents as required by Medicare to follow the rules.
Keep Updated on Policy Changes: Check for updates from Medicare and other important organizations about changes in policies, billing rules, and payment rates. Being informed will help your facility adjust and follow the rules.
⚠️ The Myth of 100 Days of Medicare Coverage in a Skilled Nursing Facility
Many people think that Medicare will pay for all 100 days of care in a skilled nursing facility. Sadly, this is often not true. Here is important information about Medicare coverage for skilled nursing facilities:
Not everyone gets the complete 100 days of coverage. If the resident stops improving in their rehabilitation, Medicare will stop coverage before the 100 days. This means that if they reach a point where no more progress is expected (i.e. they “plateau“), it will be decided that further rehabilitation will not help them get better or stay the same.
Coverage can also end if the resident refuses to participate in prescribed rehabilitation services. Medicare requires active participation for continued coverage.
Written notice must be provided when coverage is ending. The healthcare facility must give a “Notice of Medicare Non-Coverage” to tell the resident and family that coverage is ending and explain why. This notice will explain how to appeal if the resident does not agree with the decision.
Do not think that your loved one will get 100 days of Medicare coverage by default. Be sure you know what is needed for coverage. Make sure to have a plan for paying for care when Medicare stops. This could include long-term care insurance or Medicaid.
Consolidated Billing In Skilled Nursing Facilities
Under consolidated billing, Medicare requires Skilled Nursing Facilities (SNFs) to submit a single consolidated bill for most Medicare Part A services provided to patients during their covered stay. This applies regardless of whether the services are provided directly by the SNF or by an outside entity. The services included in the consolidated bill are:
- Nursing care
- Therapy services (physical, occupational, speech-language)
- Medical supplies
- Certain physician services
However, some services are billed separately under Medicare Part B coverage. These include:
- Certain dialysis services
- Certain types of chemotherapy and radiotherapy
- Services provided by outside suppliers with specialized Medicare certification (e.g., ambulance services)
It is important for SNFs to know which services go in the consolidated bill and which ones should be billed separately. If you don’t do this, your claims might be denied. For instance, if a skilled nursing facility includes ambulance service costs in the main bill by mistake, the claim might be rejected. This is because ambulance services need to be billed separately under Part B.
SNFs need to make sure they bill correctly to prevent problems with getting paid by Medicare. It is very important to understand the rules for consolidated billing. This helps to follow the law and keep things running smoothly.
🍀 Facing staffing shortages at your nursing home?
Are staffing shortages hurting your billing operations? Get dedicated billing professionals now! We will handle your nursing home workload efficiently and effectively.
Factors that Affect the Cost of Skilled Nursing Care
There are several factors that determine how much a patient should pay for skilled nursing care. These factors include:
- The state and region where the facility is located
- Whether the facility is a luxury senior living community
- The choice between a private room and a semi-private room
- The length of the patient’s stay
- The type of care required by the patient
- The patient’s insurance benefits
Boost your reimbursement now with our complete revenue cycle management services. We will ensure you get every dollar you deserve for your SNF, from eligibility verification to appeals management.
SNF
‘Billing
help is here 👨🏻⚕️