Many people on Medicare depend on durable medical equipment, such as wheelchairs, walkers, hospital beds, and oxygen equipment. When that gear wears out, Medicare Part B uses a “reasonable useful lifetime” policy, often called the 5-year rule.
In plain terms, most DME can be replaced after five years when it is no longer usable and the patient still meets medical-necessity and coverage criteria. Replacement can also happen sooner if the equipment is lost, stolen, or damaged beyond repair.
Key Points:
The 5 years are counted from the delivery date of the item to the beneficiary. This five-year period is Medicare’s “reasonable useful lifetime” for most DME.
Repairs first. During the useful-lifetime period, Medicare covers repairs when reasonable and necessary, up to the cost of replacement. If repairs will not make the item usable, replacement is considered.
When replacement is allowed. Replacement is covered when the item is worn out after its useful lifetime or if it is lost, stolen, or irreparably damaged, and the patient still meets medical-necessity rules.
Prescription and documentation. A new physician order, often a Standard Written Order, and supporting medical records are required for replacement DMEPOS.
Use in the home. The equipment must be medically necessary and primarily for use in the home to qualify under Medicare Part B DME coverage.
Supplier rules. Use a Medicare-enrolled DME supplier, ideally one that accepts assignment, or you risk paying more or getting no coverage.
No luxury upgrades. Comfort features and non-medical add-ons are not covered under DME rules.
Medicare’s five year rule for durable medical equipment means Medicare Part B will pay to replace most DME after five years from the delivery date, or sooner after loss, theft, or accidental damage, when medical necessity, documentation, home use, and supplier requirements are met.
Examples of Medicare Coverage After Five Years for DME
These simple scenarios show how the Medicare 5 year rule for durable medical equipment works in real life.
✔️ Example 1: Worn out from daily use (covered)
Situation:
James has used a manual wheelchair for six years. The wheels are worn, the seat cushion is compressed, and the brakes slip. He has used it every day at home since the original delivery date.
Action:
His physician confirms ongoing medical necessity and writes a new order. A Medicare enrolled DMEPOS supplier documents the wear and tear and prepares the claim with supporting notes.
Result:
Medicare Part B approves a replacement because the reasonable useful lifetime has passed and the chair is no longer serviceable.
Why it is covered:
RUL exceeded, continued medical necessity, and the equipment is functionally worn out.
✔️ Example 2: Repair cost is higher than replacement after five years (covered)
Situation:
Elaine’s power wheelchair is five years and two months old. The motor is failing. Repair is estimated at about $1,200 while a comparable new chair costs about $1,500.
Action:
The supplier performs a repair versus replace cost comparison and her physician confirms ongoing need for a power wheelchair. A new Standard Written Order and medical records are included.
Result:
Medicare pays for a replacement power wheelchair because replacement is more cost effective than repair and the five year period has elapsed.
Why it is covered:
Meets replacement criteria under Medicare Part B. The item is beyond its useful lifetime and replacement is the prudent option.
❌ Example 3: Five years have passed but the device still works (not covered yet)
Situation:
Victor’s walker is six years old. It squeaks and the handles look worn, but it remains stable and safe.
Action:
His physician checks the walker and confirms that it is still functional. No repairs are needed.
Result:
Medicare does not approve a replacement at this time. Age alone does not qualify the device. The walker must be non functional or not reasonably repairable, and medical necessity must still be met.
Why it is not covered:
The equipment has passed the five year mark but still meets functional use. Replacement requires wear that makes it unusable or a repair cost that is not reasonable.
What If It’s Not 5 Years Yet and The Equipment Need to Be Replaced?
You do not always have to wait five years. Under Medicare Part B’s durable medical equipment rules, early replacement can be approved when specific conditions are met.
When early replacement may be covered:
- The DME is lost or stolen, and you can provide reasonable proof.
- The DME is damaged beyond repair, for example in a house fire or car accident.
- Medical necessity continues, meaning you still meet coverage criteria for the item.
- Repair is not reasonable, such as when the repair cost is the same as or higher than a comparable replacement.
What you will need
- A new physician order or Standard Written Order for the replacement DMEPOS.
- Documentation of the event, such as a statement of loss, police report, or insurance claim for theft or accidental damage.
- Supplier notes showing why repair is not practical or cost effective.
- Proof of continued medical necessity and home use, supported by your medical records.
- A Medicare enrolled DMEPOS supplier, ideally one that accepts assignment, to process the claim correctly.
Examples of the Medicare 5 Year Rule When It Is Not Yet Five Years
These scenarios show when Medicare Part B may allow early replacement of durable medical equipment and when it will only cover a repair.
✔️ Example 1: Repair cost is higher than replacement (covered)
Situation:
Steven received a manual wheelchair three years ago. It is used daily. The frame is cracked. A repair estimate is $700, while a comparable new chair costs $600.
Action:
The Medicare enrolled DMEPOS supplier submits the repair estimate and a repair versus replace comparison. Steven’s physician confirms ongoing medical necessity and writes a new order.
Result:
Medicare approves a replacement even though only three years have passed.
Why it is covered:
Repair is not reasonable because the repair cost exceeds the cost of replacement. Medical necessity continues.
❌ Example 2: Minor fix restores function (not covered for replacement)
Situation:
Bryan’s power wheelchair has a damaged footrest after two years. The chair works well otherwise. The repair is $80. A new chair would cost about $2,000.
Action:
Bryan requests a new chair, but the supplier documents that a simple repair will restore full function.
Result:
Medicare pays for the repair, not a replacement.
Why it is not covered:
The device is still within its reasonable useful lifetime and repair is cost effective. Replacement criteria are not met.
✔️ Example 3: Destroyed in a house fire (covered)
Situation:
Richard’s wheelchair was destroyed in a residential fire after one year of use.
Action:
His physician issues a new prescription. Richard provides proof of loss, such as an insurance report and photos.
Result:
Medicare approves early replacement.
Why it is covered:
The DME is lost or damaged beyond repair due to an accident, and medical necessity continues.
When Medicare Will Not Cover DME

Medicare Part B covers DMEPOS only when clear coverage criteria are met. If medical necessity is not documented, if the item is not primarily for use in the home, or if the supplier is not Medicare enrolled, the claim is likely to be denied. Writing and billing with this in mind helps practices and beneficiaries avoid preventable denials.
Not medically necessary
Coverage requires a clinical diagnosis, supporting notes, and a valid physician order. When a clinician cannot show that the device treats or manages a condition, Medicare does not pay. For example, a wheelchair requested for comfort alone is noncovered.
Not primarily for use in the home
DME is a home based benefit. Requests that apply only to travel, errands, or outdoor activities do not qualify. When home use is documented and medically necessary, portable use outside the home can follow.
Convenience items rather than treatment
Items that simply make daily life easier are not DME. Typical examples include grab bars, room air conditioners, stair lifts, and other home modifications. These do not treat a condition and are usually paid out of pocket.
Over the counter or without a valid order
Medicare expects a proper physician order, often a Standard Written Order, and records that match the device and diagnosis. A walker or brace purchased online without a prescription is not covered, even if it seems helpful.
Supplier not Medicare enrolled or not accepting assignment
Payment is available only when the supplier is Medicare enrolled and bills correctly. Buying a hospital bed or wheelchair from a seller that does not accept Medicare can leave the beneficiary responsible for the entire charge.
Luxury or deluxe features
Medicare covers the basic model that meets medical need. If a beneficiary selects premium features that are not required, Medicare pays its share for the base item and the beneficiary pays any upgrade cost. A standard wheelchair may be approved while cosmetic add ons remain patient responsibility.
Too soon for replacement or still repairable
Most DME has a reasonable useful lifetime of about five years. If the device is within that period and can be fixed at a sensible cost, Medicare covers the repair rather than a replacement. Cosmetic wear does not qualify as a reason to replace.
Item not considered DME under Medicare rules
Some health related products are outside the DMEPOS benefit. Common examples include most hearing aids, bathroom safety items such as toilet seat risers, massage chairs, and routine shoe inserts that are not part of a diabetes treatment plan.
FAQs
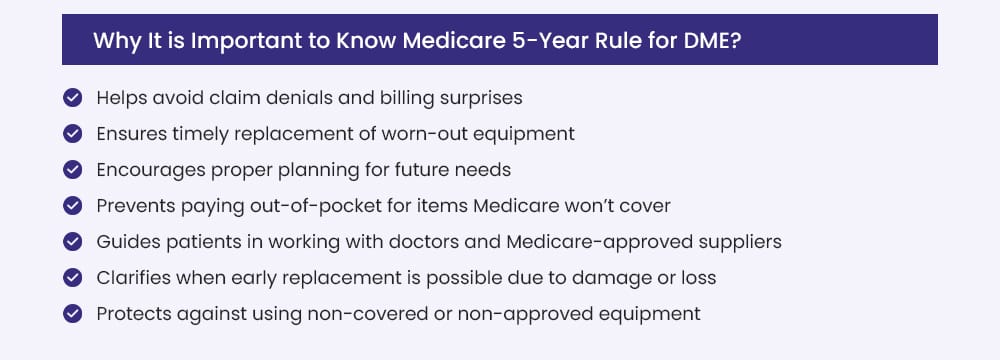
1. Why is it important to know the Medicare 5-year rule for DME?
Understanding the five year replacement policy helps beneficiaries and practices plan ahead and avoid DME claim denials. The rule affects when and how durable medical equipment can be repaired or replaced under Medicare Part B. Knowing the details reduces out-of-pocket costs and keeps care on track.
Key advantages include:
- Helps prevent claim denials and surprise bills
- Supports timely replacement of worn out equipment
- Guides planning for future DME needs
- Clarifies when early replacement may be allowed after loss, theft, or accidental damage
- Encourages working with physicians and Medicare-enrolled DMEPOS suppliers
- Reduces the risk of buying noncovered or nonapproved items
2. What is Durable Medical Equipment (DME)?
Durable Medical Equipment refers to reusable medical devices that are primarily used in the home to manage a health condition. Items must be medically necessary and appropriate for repeated use.
Common examples are:
- Wheelchairs and walkers
- Hospital beds and patient lifts
- Oxygen equipment and supplies
- Crutches and canes
- CPAP and BiPAP machines
3. What does Medicare pay?
Under Medicare Part B, payment is typically 80% of the Medicare-approved amount after the deductible. The beneficiary is responsible for the remaining 20% coinsurance. If a beneficiary has Medigap or Medicaid, that coinsurance may be covered. For many items, Medicare rents the equipment first and then may transition to ownership, following DMEPOS rules. Payment amounts and billing depend on whether the supplier accepts assignment.
Simple example
- Approved amount for a walker: $100
- Medicare pays: $80 dollar
- Beneficiary pays: $20 dollars
If a secondary plan covers coinsurance, the $20 may be paid by that plan
4. What is a Medicare-approved (Medicare-enrolled) supplier?
A Medicare-approved supplier is a company that is enrolled with Medicare to furnish and bill for DMEPOS. Using an enrolled supplier, preferably one that accepts assignment, helps ensure the claim is processed at Medicare-approved rates.
Here’s why it matters:
- Purchases from non-enrolled sellers are typically not reimbursed
- Suppliers that do not accept assignment may charge more than the approved amount
- Beneficiaries can confirm enrollment status before ordering
5. What is the reasonable useful lifetime (RUL)?
Reasonable useful lifetime is the period Medicare expects a DME item to last under normal use. For most DME, the RUL is about five years. RUL guides decisions about repair versus replacement:
- During the RUL, Medicare generally covers reasonable repairs when cost effective
- After the RUL, if the device is worn out and medical necessity continues, replacement may be covered
- Early replacement can be allowed when the item is lost, stolen, or damaged beyond repair, with appropriate documentation