Electronic data interchange (EDI) is a critical component of healthcare billing that helps streamline claims processing, reduce errors and rejections, and improve revenue cycle management. Clearinghouses are intermediaries between healthcare providers and payers, providing a single entry point for electronic claim submission and processing. However, healthcare providers need to integrate their practice management system (PMS) with their clearinghouse to realize the benefits of EDI and clearinghouses fully. Let’s discuss major components of EDI integration, its benefits and steps involved in EDI integration.
Major Components Of EDI
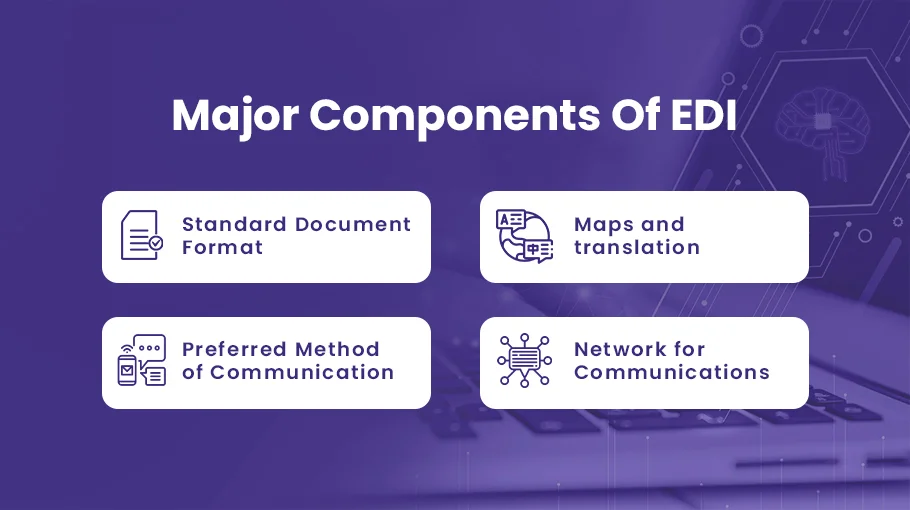
There are major components of EDI that transmit electronic data seamlessly and efficiently.
Standard Document Format
This is how data is displayed or entered into the software and how businesses share information.
Among the types of EDI data are shipping documents, invoices, and purchase orders.
Maps and translation
This comprises the software that maps the information delivered and received and translates the data. This program automates pertinent healthcare transactions and generates and sends EDI documents.
Preferred Method of Communication
Hardware for sending and receiving EDI documents is part of this communication technique. Computers, fax machines, and specialized EDI servers can all be considered EDI hardware.
Network for Communications
Different facilities and organizations can transmit and receive documents using this internet connection.
Benefits of EDI Integration in Healthcare Billing
Electronic data interchange (EDI) has become increasingly important in the healthcare industry for improving efficiency, reducing costs, and enhancing patient care. EDI allows healthcare providers to electronically submit and process medical claims instead of relying on manual processes. By integrating their practice management system (PMS) with a clearinghouse, healthcare providers can take full advantage of the benefits of EDI integration.
In this article, we will discuss the benefits of EDI integration for healthcare providers, including cost savings, improved accuracy and reduced errors, enhanced revenue cycle management, and improved patient care and satisfaction.
Cost Savings with EDI Integration
- A study by the Medical Group Management Association (MGMA) shows that practices that use EDI for claims submission experience a 40% reduction in claims processing costs compared to manual processes.
- Practices that use EDI have a 15% faster claims processing time compared to those that don’t.
- EDI allows for real-time claims processing and reduces the need for manual data entry, resulting in faster payments and improved cash flow.
Improved Accuracy and Reduced Errors
- EDI eliminates manual data entry and reduces the risk of errors and typos.
- EDI validation rules help ensure that claims are complete and accurate before submission.
- EDI edits and error reports help identify and correct mistakes and rejections in real-time.
Enhanced Revenue Cycle Management
- EDI allows for faster claims processing, resulting in improved cash flow and reduced days in accounts receivable.
- EDI enables more secured claim adjudication and payment processing, leading to improved revenue cycle management.
- EDI helps healthcare providers identify and address issues with claims processing in real-time, improving their revenue cycle management overall.
Improved Patient Care and Satisfaction
- EDI streamlines claim processing and allows for faster reimbursement, leading to improved patient care and satisfaction.
- EDI reduces the administrative burden on healthcare providers, allowing them to focus more on patient care.
- EDI provides patients with more accurate and transparent billing information, leading to improved patient satisfaction.
Steps for EDI Integration
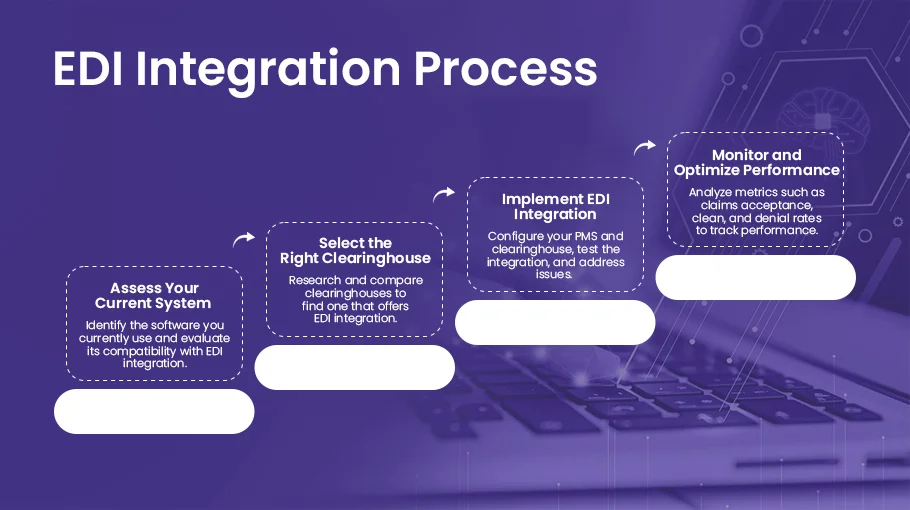
Healthcare providers must follow a few key steps to realize the benefits of EDI integration fully. These steps include assessing their current system, selecting the right clearinghouse, implementing EDI integration, and monitoring and optimizing performance.
Assess Your Current System
The first step in EDI integration is to assess your current PMS and clearinghouse software. Identify the software you currently use and evaluate its compatibility with EDI integration. Consider the features of your current system and determine areas for improvement.
Select the Right Clearinghouse
Selecting the right clearinghouse is critical to the success of EDI integration. Research and compare clearinghouses to find one that offers EDI integration options that meet your needs. Consider pricing, support, and security when making your selection.
Implement EDI Integration
Once you have selected a clearinghouse, it is time to implement EDI integration. This involves configuring your PMS and clearinghouse settings to ensure they work seamlessly together. Test the integration thoroughly and address any issues that arise. Train your staff on how to use the integrated system to maximize its benefits.
Monitor and Optimize Performance
After implementing EDI integration, it is essential to monitor and optimize performance. Track metrics such as claims acceptance, clean, and denial rates to identify improvement areas. Analyze performance data to identify trends and adjust as needed to optimize the integration.
Conclusion
EDI integration between clearinghouses and practice management systems is critical for healthcare providers to streamline their claims processing and optimize their revenue cycle management. By following the steps outlined in this article, healthcare providers can fully realize the benefits of electronic claims processing, including cost savings, improved accuracy, enhanced revenue cycle management, and improved patient care and satisfaction. Healthcare providers must stay up-to-date with technology in the healthcare industry and take advantage of EDI integration’s benefits.

