Denial Management Services

- Experts turn denied claims into recovered cash for you.
- Handling technical slips, authorization issues, and coding denials.
- Helping recover payments that might otherwise slip away.
- Smart denial management software to speed things up.
Stats of our Claim Denial Management Services
Outsource To Top-Rated Healthcare Coding Denial Resolution Service in the USA
- All Payers Supported
- Less Written Off
- Impossible Denial Flips
- Guaranteed Appeal Wins
- Minimum Denial Resolution Time
- Support with Denied Aging Claims
Get Started With A Free Quote For Your Practice →

Choosing BellMedEx Denial Management Services
Trying to manage submissions, denials, understanding claim resubmission guidelines, and maybe handling first-level appeal submissions takes time away from your patients. You shouldn’t have to wrestle with setting up denial workflow automation or solving tricky payer contract compliance rules.
That’s where our medical coding denial management service fits in. We really dig into denial management analytics and figure out the ‘why’ behind denials (denial root cause analysis) to help stop them before they start. Our job is to build smart claim denial prevention strategies for all medical specialties, clinics, and hospitals. We handle the tough stuff with denials & work to boost your first-pass resolution rate.
What clients are saying about BellMedEx

Benefits Of Our Healthcare Denial Management Service
Faster Payments
Speed up how quickly you receive money for patient services.
Fewer Rejections
Reduce the number of claims getting denied by payers.
Income Boost
Recover revenue that might otherwise be lost to denials.
Steady Flow
Create more predictable income coming into your practice.
Time Back
Free up your team's time previously spent chasing denials.
Reduced Hassle
Lessen the daily headaches caused by claim payment issues.
Clearer Trends
Gain insights into why your specific claims get denied.
Keep Up
Help manage tricky payer rules and important filing deadlines.
Better Reports
Get easy-to-understand data on denial trend and appeal success.
Insurance companies love saying no. We love making them change their minds. Even the claims you gave up on, we’ll revive them and put money back in your pocket.
BellMedEx Provides End-to-End Denial Management Solutions
Getting to the bottom of why they happen – that denial root cause analysis – is how BellMedEx’s denial management experts start building good claim denial prevention strategies. Let’s look at some common reasons claims get stuck, keeping an eye on payer-specific denial trends.

Small Slip-Ups in Patient Info?
Isn’t it maddening how tiny mistakes, like a wrong birth date or a patient’s name misspelled, lead right to a denial? These eligibility verification errors seem small but cause big hold ups in getting paid.
The solution:
Aiming for clean claims submission every time. Our denial management service catches those little errors before the claim goes out. Thanks to our advanced denial prevention tools that check medical coding information right away and prevent lots of common denials.
Getting Medical Necessity Denials from Coding Issues?
Payers check ICD-10 codes, CPT codes, and HCPCS code accuracy very carefully. Just one wrong code, maybe flagged as modifier misuse, can cause a coding denial. Keeping up with payer reimbursement policies on codes takes effort.
The solution:
Doing regular coding accuracy audits is our solid approach to manage healthcare coding denials. Making sure ICD-9 and ICD-10 codes match the care given and what payers expect cuts down on these annoying claim rejections and helps avoid flags for things like upcoding/downcoding.
Running Into Timely Filing Limit Compliance Problems?
Those claim submission deadlines feel like strict cut-offs. Send a claim past the payer’s timely filing date, and they often just won’t pay. That’s lost money just because time ran out, hurting your denial rate benchmarking.
The solution:
A good way to handle denial tracking and reporting for deadlines helps a lot. BellMedEx sets up systems to track those dates, keeping your AR (Accounts Receivable) recovery teams on track and preventing write-offs from late claims.
Sending Duplicate Billing by Mistake?
Ever had a claim denied because it looked like you sent it twice? Duplicate billing, even by accident, usually gets a quick denial. It just confuses things and delays payment for the real service.
The solution:
Good claim scrubbing before sending catches those duplicate billing issues. Our denial prevention teams double-check that each claim is accurate, preventing these easy-to-avoid denials.
Stuck with Prior Authorization Denials?
You know those services needing that pre-authorization verification green light from insurance before you do them? Missing that step often means a fast prior authorization denial. It’s a frequent spot for revenue leakage.
The solution:
Having a clear process or authorization tracking system makes sure you get that OK beforehand. This avoids those frustrating claim rejections and smooths out the financial clearance process.
Dealing with Coordination of Benefits (COB) Errors?
When patients have more than one insurance plan, figuring out who pays first can be tricky. Simple Coordination of Benefits (COB) errors cause denials and mean extra follow-up work, sometimes leaving patients with unexpected bills (patient responsibility denials).
The solution:
Using tools for benefits verification early on helps get claims to the right payer first, reducing delays caused by COB mix-ups.
Who Do We Serve?
Hospitals and Healthcare Facilities
Independent Practices & Multi-Specialty Groups
Ambulatory Surgery Centers
Diagnostic and Imaging Centers
Skilled Nursing Facilities (SNFs)
Physical Therapy and Rehabilitation Clinics
Behavioral Health Clinics
Urgent Care Centers
Plastic Surgery Clinics
How BellMedEx Denial Management Services Help Optimize Revenue Cycle?
It’s incredibly frustrating when the payment for care you delivered gets blocked by a medical necessity denial or tangled up in constantly changing payer policy updates, isn’t it? That endless cycle of ‘Fix-and-Resubmit’ drains valuable time and hits your revenue hard. We really get that grind.
BellMedEx provides specialized denial management services, acting as your partner to sort through these denials and improve your billing outcomes. Our End-to-End Denial Management Solutions aim for a higher clean claims submission rate because we are serious about coding accuracy audits and know the ins and outs of effective denial appeal services.
Focusing on Correct Codes (Coding Denial Management)
- Ensure HCPCS code accuracy.
- Address modifier misuse correction.
- Support DRG validation processes.
- Reduce coding-related denials.
Stopping Denials Proactively (Denial Prevention Strategy)
- Identify payer-specific denial trends.
- Flag missing pre-authorization verification.
- Implement claim denial prevention strategies.
- Aim to lower your overall denial rate.
- Utilize claim scrubbing software benefits.
Getting Your Earned Money Back
(Revenue Recovery & Appeals)
- Manage claim resubmission guidelines.
- Handle denial escalation protocols if needed.
- Use retrospective claim reviews to find opportunities.
- Turn denied claims into recovered revenue.
Tackling Old Balances
(RCM Denial Management Services for AR)
- Address aged claims proactively.
- Handle payment follow-up consistently.
- Provide clear denial tracking insights.
- Work on write-off reduction strategies.
- Help resolve self-pay denial issues.
Tailored Help for Different Settings (Hospital & Physician Denial Management)
- Understand Medicare / Medicaid denial patterns.
- Navigate commercial payer denial trends.
- Address setting-specific challenges, like outpatient surgery coding denials.
- Aims to maximize reimburesment across the board.
Focusing on Correct Codes (Coding Denial Management)
- Conduct thorough claim audits for accuracy.
- Implement denial workflow automation where helpful.
- Use predictive analytics for denials insights.
- Aim for Denial Management for Revenue Cycle Optimization.
- Improve your 1st attempt claim submission approval rate.
Our Denial Management Services Include
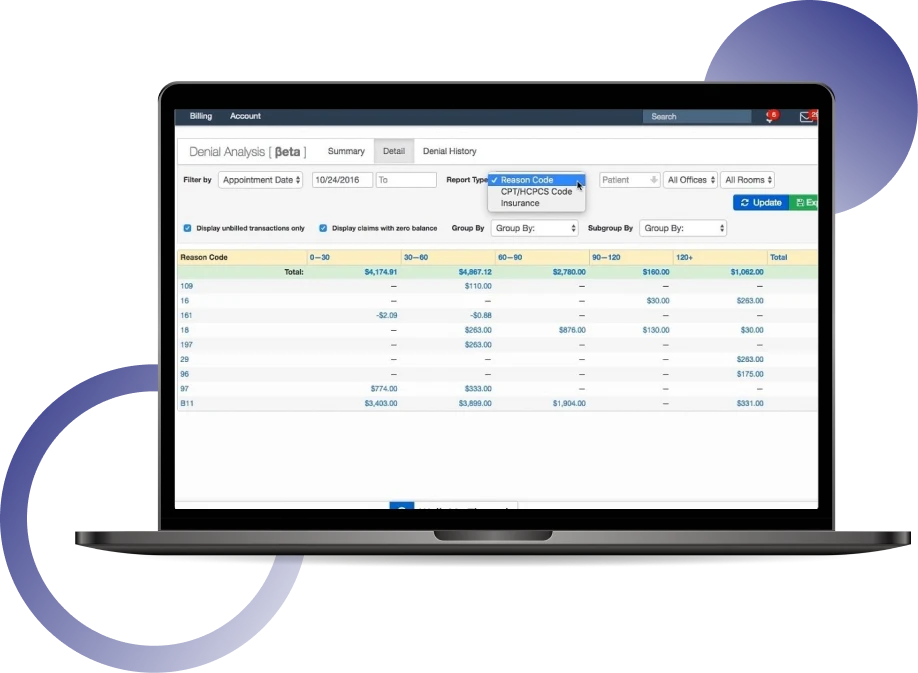
Denial Analysis
Digging into denial reasons and patterns.
Appeals Management
Handling the full appeal process for denied claims.
Coding Audits
Reviewing CPT, ICD-10, and HCPCS codes linked to denials.
Root Cause ID
Pinpointing the exact origin of claim denials.
Trend Tracking
Monitoring denial patterns by payer, department, or service line.
Prevention Strategy
Developing steps to stop common denials recurring.
Payer Follow-up
Actively contacting payers on submitted appeals status.
Authorization Support
Helping track and verify necessary patient pre-approvals.
AR Recovery
Focusing effort on aged, denied claims sitting in receivables.
Compilnce Checks
Making sure appeals follow payer and regulatory guidelines.
Performance Reports
Providing clear data on denial rates and recovery success.
Clinical Review
Assisting with medical necessity documentation gathering.
Guaranteed Payment Recovery with BellMedEx Denial Management Outsourcing Solutions
Getting a submitted claim pushed back because of a coding mistake feels like a major setback and requires focused denial management expertise. A wrong ICD-10 diagnosis code that doesn’t properly support the billed CPT procedure code leads to medical necessity denials. OR maybe just a simple CPT code mismatch can halt payments on that specific claim.
This creates rework nobody has time for and impacts your denial rate benchmarking.
We know these coding specifics really affect your daily workflow and directly hit your healthcare specialty’s income, making coding denial management services essential. BellMedEx denial management experts are centered on getting your coding accurate before each claim is sent out.
Instead of just reacting to denied claims and managing endless claim resubmissions, the BellMedEx Denial Management Service aims to help you submit cleaner patient claims consistently. Here’s how our denial management experts assist:
Smart claim scrubbing techniques:
Paper claims? Filing cabinets overflowing? Come on, it’s 2025! With EHR-integrated billing, say hello to automated claim submissions. We’re talking quick, accurate electronic claims zipping off to insurance companies at the speed of, well, the internet. Plus, you can automate appointment scheduling within your EHR.
We double-check the codes match the patient visit:
Getting modifiers right really counts:
Avoiding risky coding moves:

It’s easy to feel like you have no voice against insurance denials. We make sure you do… LOUD & CLEAR!
Our Denial Management Service Workflow
BellMedEx’s medical coding denial resolution service aims for prompt payment with a less than 2% denial ratio (means you have a guaranteed peace of mind that you are getting reimbursed for atleast 98% of insurance billing claims every day).
Spotting Denied Claims
Our Denial Management Coordinators use claim tracking systems and review remittance advice (ERAs/EOBs) carefully. This allows them to quickly flag any denied claims, kicking off the resolution steps without delay.
Sorting Out the Denials
The experienced Denial Management Coordinators then classify each denied claim. They figure out if it’s a technical issue (like medical coding errors), a clinical problem (questioning medical necessity), or administrative (maybe related to payer policy or eligibility), directing it to the right specialist path.
Finding the Real Reason (Root Cause)
Our Revenue Integrity Analysts dig deep to perform a thorough denial root cause analysis. They closely examine the denial codes, CARC/RARC messages, and specific requirements from payers to understand exactly why the claim was denied.
Tracking Trends and Reporting Back
Once the root cause is known, our Revenue Integrity Analysts track denial rates, common reasons, and other key metrics (KPIs) using revenue cycle analytics. This information helps improve internal processes and guide Coding Denial Prevention Task Forces to stop similar denials from happening again.
Appealing and Resubmitting Claims
For denied claims needing an appeal, the process involves careful preparation. Input from Clinical Denial Managers (for medical justification) and Medical Coding Compliance Officers (for coding corrections) ensures the appeal is strong and aligns with compliance rules, boosting the chance of approval.
Meeting Appeal Deadlines
BellMedex denial management service coordinators ensure appeals are submitted strictly within the timeframes set by each payer. Missing these deadlines leads to automatic rejections, so we consider timeliness a crucial aspect.
Following Up and Checking Status
Our dedicated Denial Management Coordinators and AR Recovery Teams keep close tabs on appealed claims. We use real-time claim tracking to follow up with payers, get updates on decisions, and provide any extra information needed promptly.
Handling the Tough Cases (If Needed)
For complex or high-dollar denials that resist initial appeals, our Denial Management servicing experts might conduct peer-to-peer reviews with payer physicians, or BellMedEx's payer relations specialists might step in for secondary appeals or payer-level discussions to secure a fair reconsideration.
Analysis and Feedback
Finally, we conduct strategic denial analysis. Our healthcare coding denial control experts create clear compliance reports that feed insights back into your RCM, helping medical practitioners understand trends and strengthen overall financial health.
BellMedEx CodeInsight™ Denial Management Software
This is exactly why we developed BellMedEx CodeInsight™ Denial Software. This specialized denial management software is built specifically to catch potential medical coding errors before they result in a rejected claim. It’s an automated denial management tool focused purely on coding accuracy.
- Checks ICD-10 to CPT/HCPCS links for medical necessity support.
- Applies automated checks for correct modifier usage against payer rules.
- Incorporates known NCCI edits and common commercial payer specific denial logic
- Allows setup of unique edits based on your frequent coding denials or contracts.
- Provides simple, actionable flags highlighting specific potential coding errors.
- Helps prevent inadvertent upcoding/downcoding, supporting audit readiness.
- Designed to fit smoothly within your existing EHR-integrated denial workflows.
Getting this Denial Management Software
The BellMedEx CodeInsight™ Denial Software is available as a standalone denial management solution. It has an easy integration and hooks directly into your existing medical billing workflow + connects smoothly with your EHR software.
Alternatively, if you choose BellMedEx for your full medical billing and coding services (our rates start low, at just 2.49% of monthly collections), this powerful Denial Management Software is included for you at no additional software cost. So it becomes part of the comprehensive RCM denial management services we provide.

How This Denial Management Solution Stops Coding Denials?
Claim Entered:
As soon as claim data hits your system, the BellMedEx CodeInsight™ Denial Software immediately starts its denial audit services on the coding components.
Software Checks:
The denial management software runs instant checks. It compares diagnosis codes against procedure codes (ICD-10 vs CPT/HCPCS validation), flags potentially incorrect modifier applications based on its built-in logic, and identifies patterns known to cause payer rejections. Its denial reason code mapping logic helps anticipate issues.
Pre-Clearinghouse Scrub:
Before even reaching the clearinghouse, this software has already performed a deep coding review, acting as an automated layer of claim scrubbing specific to coding rules.
Cleaner Submission:
Because the Denial Management Software flags potential coding problems for review before transmission, the likelihood of claims getting denied for these reasons drops significantly. This denial management system helps ensure coding accuracy against thousands of established rules and payer preferences.
The first denied claim you recover with us will change how you think about your business forever. Hope isn’t a revenue strategy. We build the system behind your practice that makes denials rare and recoveries routine.

Our Hospital Denial Management Services Converting Denied Claims into Approved Payments
We’re comfortable working within the complex billing structures of large healthcare systems, aiming to recover denied revenue tied up in rejected hospital claims. Our dedicated denial management team understands the hospital setting. We work closely with your various hospital billing departments – perhaps reviewing intricate claims coming from radiology, high cost surgical procedures, long inpatient stays, or high volume emergency department encounters.
And think about missing patient insurance pre-approvals for scheduled surgeries or advanced imaging. That causes so many payment hold ups in a busy hospital environment, right? So we help implement systems or checks for needed prior authorization verification before the service happens, stopping those difficult denials proactively.




And honestly it doesn’t matter where your practice is dealing with these claim troubles. If you’re facing denial fights in New Jersey, or getting claim delays in sunny Florida, working hard in California, or anywhere across the entire USA, maybe Texas or New York, we help.
Just schedule a simple, free chat. We can talk about your situation. Or call us direct for that kind of fast support at +1 888 987 6250. Seriously lets just talk and get this stuff sorted.