In the United States, the billing document, known as the CMS-1500 form, stands out as the focal point when healthcare providers, including physicians, use it to efficiently bill for the services they have rendered. This standard billing document plays a central role in healthcare settings, facilitating seamless communication with insurance companies to guarantee prompt and precise reimbursements. The form, recognized as the CMS-1500, serves as the backbone for processing physician claims, alongside those of other healthcare providers, making it an essential tool in the healthcare industry.
Introducing the CMS-1500 Form as the Healthcare Billing Document for Physicians
Meet the billing document that physicians rely on the most: the CMS-1500 form!
Named after the Centers for Medicare and Medicaid Services (CMS), it holds good importance in the world of healthcare billing in the United States.
Imagine this form as a superhero sidekick for doctors because it’s the primary paper they use to get paid for the essential healthcare services they provide. It’s like a special code that individual providers, group practices, hospitals, clinics, and billing companies all use to ask insurance companies to reimburse them for the care they give to patients.
This amazing CMS-1500 form ensures that doctors, along with other healthcare providers, can communicate with insurance companies in a smooth and organized way. It brings order and consistency to the entire billing process, making sure everyone speaks the same language when it comes to getting paid for healthcare services.
History
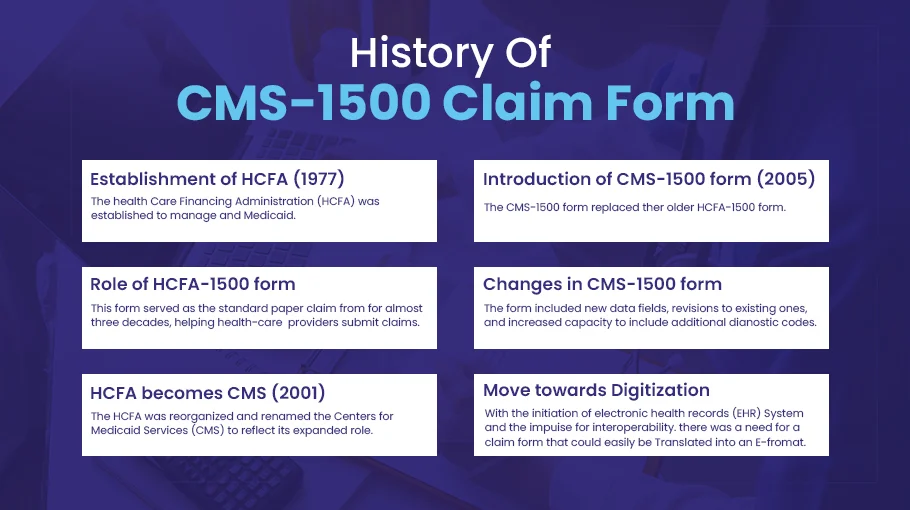
The CMS-1500 Claim Form has a history dating back to 1977 when the Health Care Financing Administration (HCFA) was established to manage Medicare and Medicaid.
HCFA introduced the HCFA-1500 form to standardize billing in healthcare. For almost three decades, it was the standard paper claim form for healthcare providers to submit claims for services to Medicare or Medicaid patients, making the process smoother and data consistent.
In 2001, HCFA became the Centers for Medicare & Medicaid Services (CMS), expanding its healthcare roles.
In 2005, the CMS-1500 form replaced the old one, accommodating changes in healthcare practices and regulations. It added new data fields and more diagnostic codes for detailed clinical reporting.
As healthcare moved towards digitization with electronic health records (EHR) and interoperability, the CMS-1500 form was designed for easy electronic data capture and exchange, a significant step in healthcare’s digital transformation.
The Ideal Billing Document for Physicians
The CMS-1500 form is the ideal document for physicians seeking seamless reimbursement for their services in healthcare billing. This form serves as a vital channel of communication between healthcare providers and insurance companies, streamlining the billing process and ensuring timely payments for the valuable care they provide.
Standardization for Effortless Billing
The CMS-1500 form was created to standardize the complex healthcare billing process. With a universally recognized structure, physicians can now easily navigate the billing process, ensuring accuracy and consistency in their claims. This standardization leads to a greater understanding among all stakeholders, resulting in smoother interactions with insurance companies.
Comprehensive Data Collection for Complete Documentation
The CMS-1500 form excels in collecting a comprehensive range of information, making it a goldmine for physicians seeking to document their patient care thoroughly. It captures essential patient demographics, diagnoses, procedures performed, charges incurred, and provider information, merging all pertinent data into a single, comprehensive form. As a result, physicians can confidently present a detailed account of their services, leaving no room for confusion during the reimbursement process.
Seamless Claim Adjudication for Swift Payments
The CMS-1500 form is essential for quick and accurate claim adjudication in the field of reimbursement. Insurance companies can efficiently validate claims and expedite the payment process for physicians by using its detailed information. Physicians can be confident that their claims will be justified and that they will receive timely and appropriate reimbursement for their essential healthcare services by providing all necessary data in a standardized format.
An Instrument for Tracking and Reporting
The CMS-1500 form serves a broader purpose in the healthcare system beyond its immediate billing function. It provides a valuable record of services rendered, which is invaluable for tracking, reporting, and analysis. This data can ultimately inform healthcare policy, planning, and research. Physicians can contribute to the advancement of healthcare practices by generating valuable insights through the data collected on the CMS-1500 form.
Usage in Healthcare Field
An extensive range of healthcare providers uses the CMS-1500 form, which includes:
Physicians and Surgeons
Doctors use the CMS-1500 form to bill for professional services, ranging from consultations and evaluations to surgeries and post-operative care.
Physical Therapists
Therapists use the form to bill for therapeutic services, including patient evaluations, treatments, and related supplies.
Chiropractors
Chiropractors use the CMS-1500 to bill for their services, including spinal adjustments, physical modalities, and other chiropractic treatments.
Outpatient Clinics
Clinics use the form to bill for various outpatient services, such as preventive care, minor surgeries, and diagnostics.
Healthcare providers use CMS-1500 to get accurate, timely reimbursements from insurers. Its standardized format makes it easier for both providers and insurers to submit and process claims.
On the other hand…
the CMS-1500 form benefits insurance companies and healthcare providers by providing a standardized format for claims. This reduces errors, facilitates processing, and ensures payments are justified.
The Framework of the CMS-1500 Form

The CMS-1500 form comprises 33 numbered blocks. Each block caters to a specific aspect of patient care and billing information.
| Block | Field Name | Field Info |
| 1 | Insurance Type | Specifies the type of insurance, including Medicare, Medicaid, or private insurance. |
| 2 | Patient’s Name | Patient’s full legal name. |
| 3 | Patient’s Birth Sex | Patient’s date of birth and sex. |
| 4 | Insured’s Name | The name of the person holding the insurance if it is not the patient. |
| 5 | Patient’s Address | Patient’s home address, city, state, zip code, and telephone number. |
| 6 | Patient Relationship to Insured | Specifies the patient’s relationship to the insured, such as self, spouse, or child. |
| 7 | Insured’s Address | The insured person’s address is different from the patient’s. |
| 8 | – | Reserved for NUCC Use |
| 9 | Other Insured’s Name | Name of any other person holding insurance that covers the patient. |
| 10 | Is Patient’s Condition Related To: | Information about whether the medical condition is related to employment, auto accident, or other accident? |
| 11 | Insured’s Policy Group or FECA Number: | Policy or group number of the insured’s health plan. |
| 12 | Patient’s or Authorized Person’s Signature: | Signature of patient or authorized person and date, granting permission to release medical information necessary to process the claim. |
| 13 | Insured’s or Authorized Person’s Signature: | Signature of the insured or authorized person, if different from the patient, giving permission to release payment to the provider. |
| 14 | Date of Current Illness, Injury, or Pregnancy: | The first date of the illness, injury, or pregnancy that necessitates the medical services billed. |
| 15 | Other Date: | Other relevant dates related to the patient’s condition or treatment. |
| 16 | Dates Patient Unable to Work in Current Occupation: | Specific dates the patient was unable to work due to the condition. |
| 17 | Name of Referring Provider or Other Source: | The name of the referring or ordering physician if applicable. |
| 18 | Hospitalization Dates Related to Current Services: | If the patient was hospitalized, the dates of hospitalization. |
| 19 | Reserved for Local Use: | Additional information as required by some insurers. |
| 20 | Outside Lab: | If lab work was outsourced and the charges associated with it. |
| 21 | Diagnosis or Nature of Illness or Injury: | The diagnosis codes related to the patient’s condition |
| 22 | Medicaid Resubmission Code/Original Reference Number: | If applicable, the code and original reference number for resubmitted claims. |
| 23 | Prior Authorization Number: | If required, the number of the prior authorization. |
| 24 | Details of the Services Provided: | Each line provides details on a single service provided including date, place, procedure code, diagnosis code, charges, and more. |
| 25 | Federal Tax ID Number: | The provider’s Federal Tax ID number. |
| 26 | Patient’s Account No: | Patient’s account number for the provider’s records. |
| 27 | Accept Assignment: | Whether the provider accepts assignment of benefits. |
| 28 | Total Charge: | Total of all charges from section 24. |
| 29 | Amount Paid: | Amount already paid, if any. |
| 30 | – | Reserved for NUCC Use |
| 31 | Signature of Physician or Supplier: | Signature of the physician or supplier including credentials and date. |
| 32 | Service Facility Location Information: | The location where services were provided. |
| 33 | Billing Provider Info & Ph. #: | Information about the provider submitting the claim. |
| 33a | Billing Provider NPI (National Provider Identifier): | The NPI of the provider submitting the claim. |
Field by Field Explanation of CMS-1500 Form
Provider Information (Blocks 24J, 32, 33)
This includes the physician or provider’s name, address, and contact details. The National Provider Identifier (NPI), a unique 10-digit number for healthcare providers, is also listed here. This information is essential to establish the identity of the service provider.
Patient Information (Blocks 1-13)
This section captures the patient’s personal and insurance information, including name, address, date of birth, gender, insurance policy number, and relationship to the insured. This information helps insurers determine the coverage and benefits applicable to the patient.
Insurance Information (Blocks 1a, 4, 11)
This section lists details about the patient’s insurance policy, including the insurer’s name, policy number, and group number, if applicable. This allows the insurance company to match the claim with the appropriate policy.
Diagnosis and Procedure Codes (Blocks 21, 24D)
These fields contain the codes assigned to the patient’s diagnoses (ICD-10 codes) and the procedures performed (CPT or HCPCS codes). These standardized coding systems help insurers understand the medical necessity of the services provided.
Other Related Details (Various Blocks)
This section captures diverse information such as the date of the medical service (Block 24A), total charges (Block 28), and the amount paid (Block 29). Any required certifications, authorization details, or referral information may also be included.
The Importance of Correctly Filling out the CMS-1500 Form
Accurately filling out the CMS-1500 form is essential for the smooth processing of insurance claims. Incorrect or incomplete forms can lead to claim denials, underpayments, or delays, which can have a direct impact on the financial health of healthcare practices. Common errors can range from administrative oversights such as misspelled names or transposed digits in policy numbers to clinical mistakes such as using outdated or incorrect diagnosis or procedure codes. A careful approach to completing the form, aided by a strong understanding of billing rules and coding conventions, is essential to avoid these consequences.
Role of Clearinghouses in the Process
In the medical billing process, clearinghouses act as intermediaries between healthcare providers and insurance companies. Once a CMS-1500 form is completed, it is typically sent to a clearinghouse. It is then scrubbed, which involves checking the form for errors, inconsistencies, or missing information. Minor errors are corrected, and the form is converted to the appropriate electronic format. The scrubbed claim is then sent to the insurance company. By facilitating error detection and correction, clearinghouses streamline the billing process, expedite claim settlements, and ultimately improve revenue cycle efficiency for healthcare providers.
Need Help with CMS-1500 Form Submission? Here’s How Bell MedEx Helps:
Bell MedEx follows a series of well-defined steps to complete and submit a CMS-1500 form for their claims.
Step #1: Patient Check-in and Information Collection
At this initial stage, Bell MedEx gathers all necessary demographic and insurance information from the patient. This may include verifying the patient’s identity, confirming insurance coverage, and stating the primary reason for the visit of patients.
Step #2: Medical Examination and Coding
Once the patient’s consultation is complete, the physician or healthcare provider determines the necessary procedures and services provided. These services are then translated into medical codes using standard coding systems like the International Classification of Diseases, 10th Revision (ICD-10) for diagnoses, and the Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) for procedures.
Step #3: Form Completion
After coding, Bell MedEx fills out the CMS-1500 form, capturing information in several key areas:
- Patient demographics and insurance information
- Provider information, including the National Provider Identifier (NPI)
- Details of the patient’s diagnoses and treatments, represented in ICD-10 and CPT/HCPCS codes, respectively
- Date of the medical service and charges for the procedures performed
Step #4: Claim Submission to Clearinghouse
After the CMS-1500 form is filled out, it is sent electronically to a clearinghouse. This entity checks the form for any error or omission, often called “claim scrubbing.” Once verified, the Fusion EDI clearinghouse sends the cleaned claim to the insurance company.
Step #5: Insurance Adjudication and Payment
The insurance company reviews the claim, a process known as claim adjudication. If the claim is approved, they issue payment based on the patient’s coverage and the provider’s contracted rates. In case of denial, an explanation of benefits (EOB) is sent, outlining the reasons for the denial.
Step #6: Patient Billing
If there’s any balance remaining after the insurance payment, which could be due to deductibles, co-insurance, or non-covered services, Bell MedEx bills the patient directly.
By adhering to this process, Bell MedEx ensures accurate, efficient, and timely claim submissions, optimizing healthcare practices’ Revenue Cycle Management and ensuring financial health.
Do you need help with CMS-1500 form submission for physician claims?
Contact us today at 888-987-6250 or request a free demo.