Key Takeaway:
Non-credentialed physicians can legally see patients under specific circumstances: when granted temporary/provisional status, under supervision by a credentialed provider, during emergencies, as out-of-network providers (with higher patient costs), or via telemedicine with appropriate cross-state licensing. However, without credentialing, providers risk reimbursement denials from insurance companies like Medicare, potential out-of-pocket costs for patients, and serious compliance and liability issues.
Imagine you’re running a healthcare practice, and a new physician joins your team. They’re experienced, talented, and eager to start helping patients.
However, there’s a hiccup—they haven’t been credentialed yet. Now, the clock’s ticking, and you’ve got patients to see.
What do you do? Do you hit pause until the credentialing process is complete, or is there a way to move forward?
It’s a scenario many healthcare providers face, and while it may seem like a sticky situation, it’s not all doom and gloom.
There are some ways to navigate these waters, and it’s essential to understand the dos and don’ts to keep things running smoothly.
Credentialing is a big deal. It’s how medical professionals get recognized and reimbursed by insurance companies like Medicare.
Essentially, the stamp of approval says, “Yes, this provider meets the necessary standards to offer services safely and effectively.”
Without it, patient safety and the integrity of the healthcare system could be at risk.
But here’s the kicker:
What happens if that new physician isn’t credentialed yet, and you need to see patients anyway?
It is a very critical situation, but the truth is, there are temporary solutions that can keep your practice moving forward.
Let’s see when and how a physician can see patients without being credentialed.
What Does It Mean to Be Credentialed?
Credentialing is the process where healthcare providers, like doctors, nurses, or specialists, are verified for their qualifications.
This process involves reviewing a provider’s education, training, licensing, malpractice history, and work experience to ensure they meet the standards of the healthcare institution and are eligible for insurance reimbursements.
While credentialing is typically a standard process for doctors, nurses, and other healthcare professionals, sometimes there is a delay between when a provider joins a new facility or health plan and when their credentialing is officially completed.
If a physician isn’t credentialed, they can’t officially bill insurance companies, including big players like Medicare.
Without that credentialing stamp of approval, they’re not recognized as a valid provider under those insurance contracts.
This can lead to a few complications:
First, you won’t be reimbursed for the services provided, and second, it could even raise concerns about compliance and patient safety, depending on the situation.
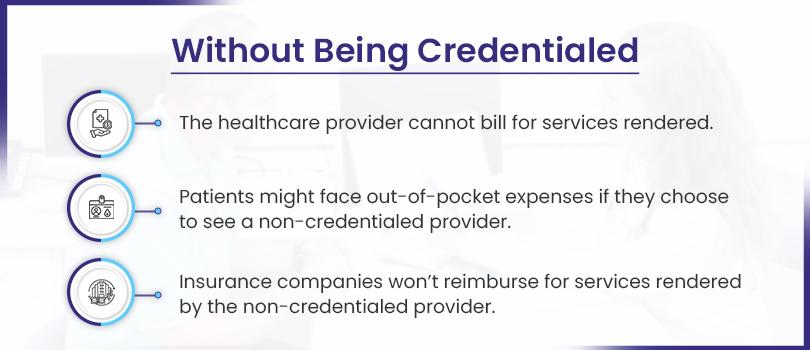
Without credentialing, health plans, including Medicare, Medicaid, or private insurers, don’t recognize a provider.
This means that:
- The provider cannot bill for services rendered.
- Patients might face out-of-pocket expenses if they choose to see a non-credentialed provider.
- Insurance companies won’t reimburse for services rendered by the non-credentialed provider.
Can Non-Credentialed Providers See Patients: Potential Risks
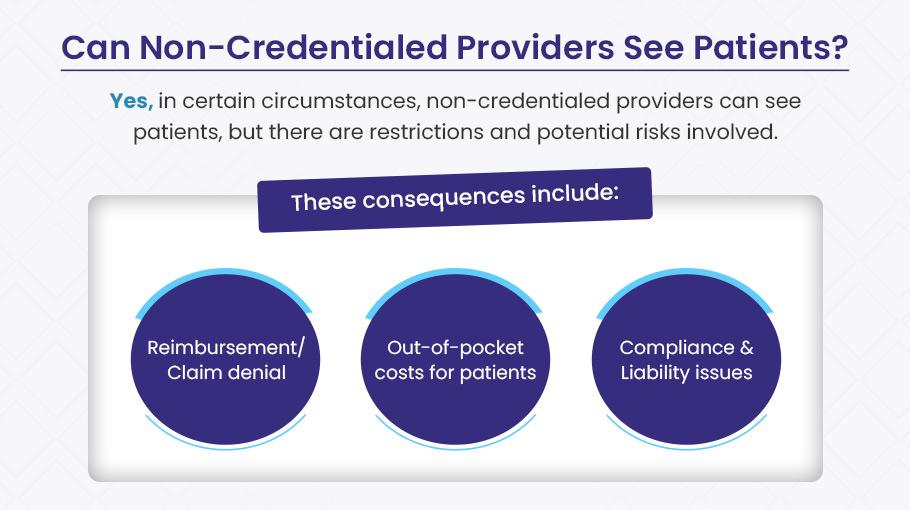
YES, in certain circumstances, non-credentialed providers can see patients—but it’s not as simple as just letting them dive in.
There are significant restrictions and potential risks involved that you need to consider before allowing any provider to treat patients without full credentialing.
Everything runs on high standards, strict protocols, and paperwork in healthcare.
Why?
Because patient well-being, legal obligations, and the financial health of a healthcare organization all depend on it.
Credentialing plays a considerable role in this system. It ensures that a provider meets specific qualifications and standards to safely treat patients and be authorized to bill insurance companies, including large payors like Medicare and private insurers.
But what happens when a provider isn’t credentialed yet and still sees patients?
Well, here’s where things get tricky.
Allowing a non-credentialed provider to see patients before completing the credentialing process can open the door to several risks that could harm your practice financially and legally.
Let’s take a closer look at these risks:
1). Reimbursement Denial
One of the most significant risks of seeing patients before completing the credentialing process is the potential for reimbursement denial.
Insurance companies, including major payers like Medicare and private insurance providers, have strict rules regarding credentialing.
They typically require that healthcare providers are officially credentialed and authorized before any services are eligible for reimbursement.
Insurers require that healthcare providers meet specific qualifications and have the necessary approvals before they are eligible for reimbursement.
Without proper credentialing, any services provided will likely be denied payment.
If a provider has seen patients without credentialing approval, they cannot collect payment for the services rendered until their application is processed.
This could lead to significant financial challenges for the practice, especially if the provider has seen many patients.
Example
A newly hired physician begins seeing patients at a practice while awaiting credentialing approval from Medicare.
His application is under review, but he provides services and bills Medicare for the visits.
Since he is not yet credentialed, Medicare denies the reimbursement. The physician and his practice now face a situation where they have provided care but will not receive compensation for the services offered.
Providers should not assume that reimbursement will be granted while waiting for credentialing approval.
Until the credentialing process is complete, they should refrain from submitting claims to insurance providers.
2). Out-of-Pocket Costs for Patients
Patients typically rely on their insurance coverage to help pay for medical services.
If a provider is not credentialed with the patient’s insurance, patients may be required to pay out-of-pocket for the services they receive.
This can create several problems for both the patient and the provider.
Insurance companies generally won’t reimburse for services rendered by non-credentialed providers.
As a result, patients will likely be responsible for the full cost of their care, which they may not have budgeted for.
Most patients expect their medical expenses to be covered by their insurance.
When faced with unexpected costs because their provider isn’t credentialed, it can lead to frustration, dissatisfaction, and even a loss of trust in the provider.
This can result in a negative impact on patient retention and the provider’s reputation.
Example
A patient visits a specialist, and doctors assumes that his insurance will cover the costs of the consultation.
However, the physician is not yet credentialed with the patient’s insurance provider, so they must pay out-of-pocket.
Upset by the unexpected expense, the patient might seek treatment elsewhere, potentially losing a patient for the doctor.
Non-credentialed providers may lose business due to patients refusing to pay out-of-pocket for services. Healthcare providers must ensure that their credentialing process is complete before seeing patients to avoid placing this financial burden on them.
3). Compliance and Liability Issues
Seeing patients without the necessary payer credentialing poses a significant legal risk, including compliance and liability issues.
Providers who fail to adhere to proper credentialing protocols may face legal challenges, especially if something goes wrong during care provision.
If a non-credentialed provider is involved in a malpractice case or any legal issue, they may find themselves without legal protection or coverage under their malpractice insurance.
This could leave the provider personally liable for the financial and legal consequences.
Healthcare organizations must comply with various regulations, including credentialing-related ones.
Providing services without completing the credentialing process could be seen as a violation of these regulations.
Failure to comply with credentialing requirements could sometimes lead to fines, sanctions, or even the termination of a provider’s license.
Physicians who see patients before their credentialing is complete take on considerable legal and financial risks. Malpractice claims, insurance issues, and violations of healthcare regulations could jeopardize their practice and professional standing.
Example
Suppose a doctor is not yet credentialed with the insurance provider and decides to treat a patient for a routine procedure.
During the procedure, a complication arises, and the patient sues the doctor for malpractice.
Since the physician wasn’t credentialed, the malpractice insurance policy might not cover his legal defense costs or any potential settlement, leaving him personally responsible for those costs.
When Can a Non-Credentialed Provider See Patients? Key Scenarios Explained
While proper credentialing is a cornerstone of healthcare compliance and reimbursement, there are specific circumstances where providers can legally see patients before their credentialing process is complete.
These exceptions provide necessary flexibility in the healthcare system while maintaining patient safety standards.
We’ve outlined the key scenarios below where providers may be permitted to practice prior to full credentialing approval:
✅️ Temporary Credentialing or “Provisional” Status
Sometimes, a provider may be granted temporary or provisional credentialing to see patients while the complete credentialing process is underway.
This is commonly seen when a physician joins a hospital or practice and needs to start seeing patients immediately, even if their full background check isn’t completed yet.
From an insurance perspective, provisional status can lead to service reimbursement, but it’s not guaranteed.
For example, Medicare might reimburse for the care a temporarily credentialed physician provides, but this arrangement is typically short-term and subject to various conditions.
What to Keep in Mind?
Provisional status doesn’t guarantee reimbursement, and there can be delays of weeks or months before full credentialing is approved.
If the provider’s provisional status expires before the credentialing is finalized, they might not get paid, and patients could be on the hook for the charges.
✅️ Supervision by a Credentialed Provider
A non-credentialed provider may be able to see patients if they are working under the supervision of a credentialed provider.
This is common for non-physician providers, such as nurse practitioners (NPs) or physician assistants (PAs), who work under a supervising physician.
Let’s say a Nurse Practitioner is in the process of being credentialed by Medicare but has already started working at a primary care clinic.
While the nurse waits for her credentials, she may see patients if her supervising physician is present or available to oversee her care decisions.
When it comes to insurance, Medicare and other insurers typically reimburse the credentialed supervising provider for services rendered.
This means that while the supervising physician can bill for the care provided, the non-credentialed NP won’t be reimbursed directly.
The supervision arrangement ensures that the supervising physician remains legally responsible for the care provided and that billing is tied to the supervising physician’s credentials.
What to Keep in Mind?
Clearly understand that non-credentialed providers can’t bill independently; the supervising physician’s credentials will be used for the billing process.
This supervision arrangement can extend to the billing process, so patients might not notice a difference, but the financials behind the scenes can be a little more complex.
✅️ Emergency or Unforeseen Circumstances
There are situations in which emergency care or urgent needs arise, and a non-credentialed provider may be the only one available to treat patients.
In these cases, insurance companies like Medicare has specific emergency services and coverage guidelines.
For example, a doctor is not yet credentialed with Medicare but works in an urgent care facility.
One day, an unexpected influx of patients requires her to step in and see a patient with a complex condition.
While they are not credentialed, the facility calls her in due to the emergency, and she provides care.
For emergencies, Medicare and most other insurers will generally cover care provided by a non-credentialed provider.
This is because patient health and safety are prioritized in emergencies, and credentialing delays are recognized as an administrative issue.
What to Keep in Mind?
The services rendered must be truly emergent or urgent. If the care is routine or non-urgent, reimbursement may be denied for non-credentialed providers.
Medicare has strict guidelines about what constitutes an “emergency,” and this can vary by case. Providers need to ensure they document everything accurately.
✅️ Out-of-Network Providers
In some instances, a non-credentialed provider may not be in-network for an insurance plan, but patients may still be able to see them as out-of-network providers.
The patient would typically be responsible for a higher out-of-pocket cost, but the insurance may offer partial reimbursement.
For instance, a specialist who isn’t credentialed with a specific insurance company.
However, he agrees to see a patient who has that insurance.
The patient might still be able to get some reimbursement from their insurance provider, but it will likely be at a reduced rate, and they may need to pay higher co-pays or deductibles.
Medicare, for example, has a network of approved providers, but it does not allow patients to see out-of-network doctors.
However, if the provider is non-credentialed, reimbursement will likely be limited or unavailable, and patients might have to pay the full cost.
What to Keep in Mind?
Patients will typically have higher out-of-pocket costs when seeing out-of-network or non-credentialed providers.
Explaining the financial situation to patients upfront is essential so unexpected bills don’t blindside them.
✅️ Telemedicine and Cross-State Licensing
With the rise of telemedicine, non-credentialed providers might also encounter questions related to cross-state licensing or telehealth provisions.
A physician who isn’t credentialed in a particular state may still offer services via telemedicine to patients in that state.
For example, a licensed physician in Texas hasn’t yet been credentialed by an insurance provider in Louisiana.
However, she offers telemedicine consultations to patients in Louisiana, raising the question of whether Medicare will reimburse those services.
Many insurance companies, including Medicare, are adapting to the rise of telemedicine.
Reimbursement policies are evolving, but if a provider is often licensed in the state where the patient is located, they may still be able to offer telehealth services, even if they are not yet credentialed with the insurance provider.
What to Keep in Mind?
The rules around telemedicine and cross-state licensure vary by insurance company and state. It’s crucial to check each payer’s specific guidelines before proceeding.
Credentialing requirements may differ for telemedicine services, and even if credentialing is pending, reimbursement may still be possible in some cases.
Become a Credentialed Provider with BellMedEx
BellMedEx, a top USA healthcare company, simplifies billing, RCM, and credentialing. Our medical credentialing services help physicians meet insurance and regulatory requirements smoothly. Contact us today to enroll as a credentialed provider and enhance your practice with ease.