The Trusted ABA Billing Services Company
As a full-service ABA therapy billing services provider, we handle everything from insurance credentialing and telehealth billing to EMR integration, claims scrubbing, and denial prevention. Plus, we ensure every claim aligns with Medicaid, Medicare, and private payer rules.
Fill out the form below to let BellMedEx’s trusted ABA revenue cycle management solutions streamline operations and maximize revenue for your practice.
Trusted ABA Medical Billing Solutions for every therapy:
Initial Assessments and Evaluations
Individual ABA Therapy Sessions
Group ABA Therapy Sessions
Parent and Caregiver Training
Telehealth ABA Services
Behavioral Assessments and Data Analysis
Behavioral Assessments and Data Analysis
Crisis or Emergency Intervention Services
Speech-Language Pathology (SLP)
Occupational Therapy (OT)
Providing Customized ABA Therapy Billing Services in the USA
For 10+ years, BellMedEx ABA Therapy Billing and Collections Company has worked with ABA providers to turn their ABA medical billing from a problem into a profit source.
We take full control of your revenue cycle rather than just managing it. Our team includes certified AAPC coders and RCM experts who solve ABA billing challenges like checking claims for proper diagnostic codes, fixing denials in as less as 48 hours, and working with ABA insurance payers to get you better rates.

End-to-End Ownership:
From prior authorizations to self-pay collections—we handle every touchpoint.
Proprietary Denial Resolution Framework:
Fix recurring issues like COB errors or modifier misuse for good.
Live Claims Tracking Portal:
Watch claims move from submission to payment in real time.
Revenue Growth Guarantee:
We benchmark your pre- & post-partnership revenue—or we work free until we fix it.
95% Denial Resolution Rate:
Via aggressive appeals and modifier optimization.
What are ABA Billing Services?
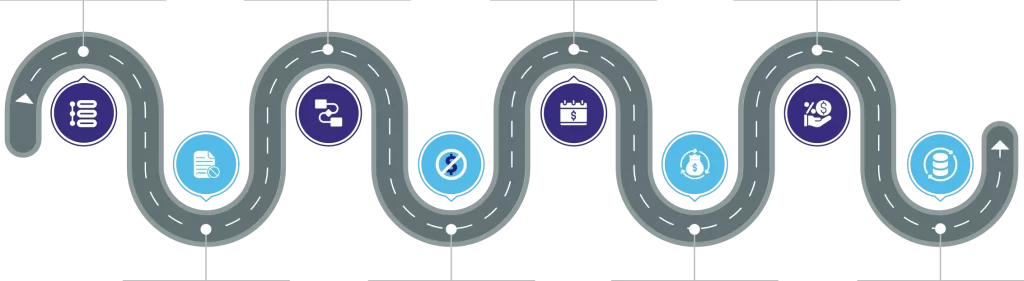
The core components of ABA Therapy Billing Services are:
- Insurance Verification and Benefits Analysis
- Verifying patient insurance coverage for ABA therapy
- Determining in-network vs. out-of-network benefits
- Calculating patient financial responsibility
- Prior Authorization Management
- Submitting documentation to prove medical necessity
- Tracking authorization periods and units
- Managing reauthorization processes before expiration
- Precise Coding and Documentation
- Utilizing appropriate CPT codes (97151, 97153, 97155, etc.)
- Applying necessary modifiers (TM, TS, 59)
- Ensuring accurate ICD-10 diagnostic codes (F84.0, F84.5)
- Verifying proper documentation to support billed services
- Claims Submission and Follow-up
- Electronic submission of claims within timely filing limits
- Tracking claim status and payment timelines
- Implementing claim scrubbing to reduce rejection rates
- Denial Management and Appeals
- Analyzing rejection reasons and patterns
- Correcting and resubmitting denied claims
- Filing formal appeals when necessary
- Revenue Cycle Analytics
- Generating financial performance reports
- Analyzing reimbursement trends and payer behaviors
- Identifying opportunities for process improvement
- Compliance Management
- Ensuring adherence to payer-specific requirements
- Maintaining HIPAA compliance in all billing practices
- Staying updated on changing regulations affecting ABA reimbursement
Therapists Trust BellMedEx ABA Therapy Billing and Collections Company for Many Reasons

Unmatched ABA Billing Expertise
Our team brings decades of combined experience exclusively in billing ABA therapy services. Unlike general medical billers, we understand the unique complexities of ABA service delivery models, authorization management, and the specific documentation requirements that make ABA billing different. This specialized knowledge translates directly to higher clean claim rates and faster payments for our clients.

98.7% First-Pass Claim Approval Rate
Our track record speaks for itself. While the industry average hovers around 70%, our clients consistently experience first-pass approval rates of 98.7%. This remarkable difference isn't by chance. It's the result of billing ABA services with excellent claim preparation, thorough understanding of payer requirements, and proactive verification processes that catch potential issues before submission to the payor.

Rapid Revenue Acceleration
When practices switch to BellMedex ABA insurance billing services, they see a huge reduction in their reimbursement timeline. Your practice will no longer wait several months for ABA insurance payments. Our streamlined processes and payer relationships help secure payment within a few days of claim submission. This dramatically improves the cash flow of ABA clinics.

ABA-Specific Denial Prevention System
We've developed a proprietary denial prevention system specifically for ABA claims that identifies and resolves the top issues before they become problems. This system has reduced denial rates for our clients by up to 78% compared to their previous billing solutions, eliminating the frustrating resubmission cycle that delays your payments.

Compliance Guarantee
Our team stays continuously updated on the ever-changing landscape of insurance requirements, state regulations, and ABA coding guidelines. We offer a compliance guarantee that protects your practice from audit concerns while ensuring you receive every dollar you're entitled to—legally and ethically.

Customized Client Portal
Our secure, HIPAA-compliant client portal gives you 24/7 visibility into your ABA billing operations. Track ABA medical billing claims in real-time, access comprehensive financial reports, and gain actionable insights into your practice's financial health with just a few clicks. This transparency builds confidence and eliminates the uncertainty that often comes with outsourced billing.

Dedicated ABA Account Specialists
Every practice gets their own billing specialist who gets to know you and your needs. This person becomes familiar with how you work, which insurance companies you deal with, and what your goals are. Having your own helper means you always know who to call when you have questions.

Works With Your Current EMR System
Our billing system connects easily with the software you already use in your practice. This means no double-entry of information and less paperwork for your staff. Our clients save about 15 hours each week on admin work, that's almost two full workdays!

Proven Revenue Impact
ABA healthcare providers experience up to 30% increase in collected revenue after their partnership with our ABA Billing and Collections Company. This dramatic improvement comes not just from better claim management, but from our comprehensive approach to revenue cycle optimization that identifies previously missed billing opportunities.
- ABA Therapy Clinics/Centers
- Small Group ABA Practices
- Pediatrics/Developmental Departments
- Multidisciplinary Pediatric Clinics
- Autism Treatment Centers
- Early Intervention Providers
- Community Mental Health Centers
- Residential Treatment Facilities
- Behavioral Needs Group Homes
Why Do ABA Healthcare Practices Need Medical Billing and RCM Services?
| Without ABA Billing Services | With ABA Billing Services |
|---|---|
| Billing codes keep changing. You can’t keep up! ABA billing codes and insurance requirements frequently shift. Missing updates can lead to claim rejections or underbilling. | Imagine having someone whose entire job is to stay on top of these changes. That's what you can expect from ABA billing service providers. They’ll handle the fine print so your claims match what insurers expect right now, not six months ago. |
| My team misses small details in notes, and claims get denied. It happens. When you’re focused on client care, it’s easy to skip a time note or forget a progress update. Even tiny gaps in paperwork can hold up payments for weeks. | ABA billing specialists review documentation for accuracy & completeness, flagging gaps before claims are submitted. This reduces denials tied to paperwork issues. |
| Insurance authorizations take too long. Delays in prior authorization approvals stall services and payments. Calling insurers, resending forms, worrying about coverage gaps… it’s a time sink that pulls you away from your clients. | ABA billing service providers have a proactive authorization management that ensures treatment plans and progress reports are submitted early, with follow-ups to avoid lapses in coverage. |
| High claim denial rates. Errors like incorrect patient details, mismatched codes, or missing provider signatures result in denials that drain resources to fix. | ABA billing companies catch errors upfront (like a second set of eyes) and fix denied claims fast. Plus, they’ll tell you why it happened, so it doesn’t repeat. |
| Limited understanding of ABA-specific billing rules. ABA isn’t one-size-fits-all. General billers might miss nuances like timed units, specific modifiers, or how insurers interpret “medical necessity” for autism care. This leads to underpayments. | Dedicated ABA billers understand these intricacies, ensuring claims meet each insurer’s criteria for timely, full reimbursement. |
| ABA insurance reimbursements are slow, cash flow feels unpredictable. Submitting claims late or failing to track their status delays cash flow, affecting your practice’s financial health. | ABA medical billing company streamlines submissions, tracks every claim in real time, and gently hassles insurers about delays. Predictable cash flow = less financial anxiety. |
Trust Our 10+ Years Of Expertise in ABA Therapy Coding
You collaborate directly with specialists who understand ABA’s unique challenges.
We Know ABA Codes Perfectly
Following Rules Is Our Priority
We Know Each Insurance Company's ABA Rules
Proper Money Management
ABA-Focused Coding Support


BellMedEx Delivers ABA Insurance Billing Services Across The USA
BellMedEx ABA Insurance Billing Services Company manages the complete billing process – from verification of benefits to claims submission and follow-up – making sure every medical service you provide to patients is properly documented and reimbursed according to each specific insurance company’s requirements.
We successfully process claims with all major insurance providers covering ABA therapy, including:

Is your ABA agency claiming 9% extra Medicare reimbursements via BellMedEx?
- We access your billing systems and pull data on client outcomes, session notes, and all quality measures specific to ABA therapy services.
- We monitor Cost category performance to prevent negative adjustments.
- Our team reviews your data against MIPS benchmarks. If you are falling short in quality scores or technology use, we flag them early and take steps to resolve them for you.
- We handle all reporting deadlines and audit trails. Post-submission, we track Medicare’s feedback on your ABA clinic’s performance and adjust MIPS optimization strategies proactively.
- We ensure your ABA EHR usage meets Promoting Interoperability requirements.

- A 9% Medicare cut hurts. We make sure it never happens.
- Top performers earn up to 9% bonuses. We optimize reporting to position you competitively.
- We know how MIPS judges ABA progress data, and we report codes like HCPCS 0362T correctly. This way, you can redirect the hours you spend on MIPS compliance back to therapy sessions.
- We handle the final submission and verify acceptance by Medicare—no extra work on your end.

You’re good at therapy. But MIPS isn’t about therapy… it’s about data rules, right? One coding mistake or missed deadline can cost thousands. We’ve fixed $1.2M in penalties for ABA clinics in the past two years.
Let’s talk for 10 minutes. We’ll show you your current MIPS score and
what’s at stake. No contract. No pressure.
Need an Expert & Trusted ABA RCM Support?
Behind every life-changing ABA session is a billable moment. That’s why, BellMedEx ABA Therapy Billing Services Company works as your financial co-therapist that injects predictability into your RCM.
Our ABA revenue cycle management solutions promise real-time eligibility checks, rewire denials into paid claims, sync payments from patients and health insurance companies to your payroll cycle, and turn AR aging reports into recovery roadmaps.
Streamline eligibility verification with real-time insurance checks to prevent ABA therapy claim rejections upfront
Automate ABA billing workflows for error-free claims submission, payment posting, and reconciliation across private payers & Medicaid
Boost patient collections via customized payment plans, automated reminders, and HIPAA-compliant online portals
Prevent revenue leaks with monthly compliance reviews for ABA coding (e.g., adaptive behavior codes), billing regulations, and payer updates
Slash ABA claim denials through proactive coding audits and payer guideline alignment
Who is BellMedEx?
BellMedEx emerges as the USA’s #1 trusted ABA billing services company, purpose-built to transform the administrative landscape of behavioral therapy practices. Our end-to-end ABA billing solutions are a lifeline for therapists drowning in paperwork, offering a comprehensive approach that maximizes revenue, ensures compliance, and eliminates billing-related stress.
With BellMedEx, ABA practices can finally shift their full attention from bureaucratic challenges to providing compassionate, effective behavioral support. This way ABA therapists can better serve children with autism.
Direct Benefits to Your Practice
Seriously, who understands all those ABA codes and rules? We do. Our certified ABA billing team knows exactly how to talk to insurance companies. We’ll code claims right, chase denied payments, and squeeze every penny insurance owes you.
Get Paid More
With our top-rated ABA RCM (Revenue Cycle Management) services, we streamline everything from insurance verification to payment posting. BellMedEx chases down every penny insurance owes you, fights denied claims, and fixes underpayments as part of our ABA insurance billing services.
No More Insurance Surprises
Tracking ABA payments without BellMedEx feels like solving a Rubik’s cube blindfolded. But don't worry. BellMedEx ABA Therapy Billing and Collections Company will show ABA practices where their reimbursements are, post payments fast, and send friendly payment reminders to patients who owe co-pays and deductibles. Authorizations are also handled here, so there are no treatment delays. And if auditors come knocking? BellMedEx has got your back. HIPAA rules? We handle them.
Reliable ABA Billing Support
Other billing companies treat you like a number. BellMedEx treats ABA providers like family. Text us at 2 AM with a billing panic? We’ll answer. Need help understanding a weird insurance letter? We’ll translate it. Outsource ABA billing operations to us, and we will be here for you always.



