Introduction
Inaccurate coding and billing in healthcare can lead to severe consequences. When healthcare providers submit false claims, they put their financial stability at risk. This leads to accusations of medical abuse and fraud. They may face fines and penalties from the government.
This article discusses the pitfalls arising from inaccurate coding and billing in healthcare. It also emphasizes the risks healthcare providers face. These risks include financial losses, legal consequences, damage to reputation, and unreliable patient-provider relationships. By understanding and addressing these issues, healthcare providers can minimize their negative impact and ensure overall better patient care.
Pitfalls of Inaccurate Coding and Billing
Inaccurate coding and billing lead to complications of abuse and fraud according to Healthcare FCA. Healthcare frauds include upcoding of services, unbundling, and deceiving the insurer in any manner. Knowingly submitting false claims implements severe illegal consequences that must be combated right away.
Financial Losses and Penalties
Inaccurate coding and billing can result in financial losses and penalties for healthcare providers. Submitting false claims to the government can lead to hefty fines and may even threaten the financial stability of healthcare institutions. Penalties under the Federal Civil False Claims Act (FCA) can be severe, with the potential for recovery of up to three times the amount of damages sustained by the government.
A 2018 American Medical Association (AMA) study found that medical billing errors lead to an average loss of approximately 7% of a physician’s total annual revenue. These errors can result from inaccurate coding, including upcoding (assigning higher-cost codes to inflate reimbursements or under-coding .Other billing errors include duplicate billing and unbundling of services, which can lead to denied claims, underpayments, or overpayments.
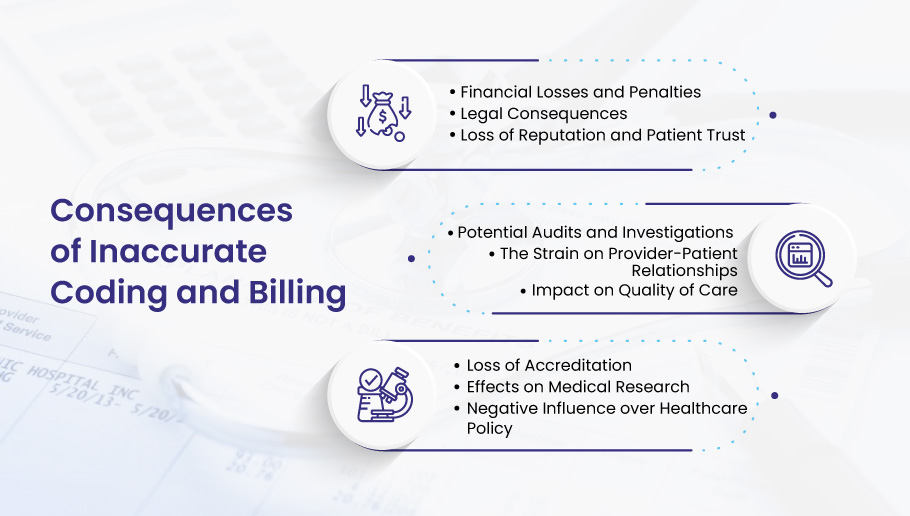
Legal Consequences
Apart from financial penalties, legal consequences can arise from inaccurate coding and billing. Violating the Federal Civil False Claims Act can result in imprisonment, tarnishing healthcare providers’ reputations, and damaging their patients’ trust.
Inaccurate coding and billing can lead to legal ramifications for healthcare providers. For instance, in 2018, a hospital in Florida agreed to pay $85 million to settle a lawsuit alleging fraudulent billing and Stark Law violations related to physician referrals. In another example, a Texas-based healthcare system consisting of fifteen doctors agreed to pay $2.83 million in 2020 to resolve False Claims Act allegations related to improper billing and upcoding.
Loss of Reputation and Patient Trust
When healthcare providers are found guilty of medical abuse or fraud, their reputations are often irreparably damaged. This can lead to the loss of patient trust, which is essential for the continued success of a healthcare institution. Patients may seek care elsewhere, resulting in a decline in patient volume and revenue.
Inaccurate coding and billing can lead to reputational damage for healthcare providers, affecting patient trust, referrals, and overall revenue. In a 2019 survey by the Kaiser Family Foundation, 67% of respondents reported concerns about unexpected medical bills, with 55% indicating that they had lost trust in their healthcare provider due to billing issues. Negative press coverage, regulatory sanctions, and word-of-mouth can all damage the public image. Thus making it harder for healthcare providers to attract and retain patients.
Potential Audits and Investigations
Healthcare providers who engage in inaccurate coding and billing may be subjected to audits and investigations. These can be time-consuming, costly, and disruptive to normal operations. Audits and inquiries can also lead to further financial penalties and legal consequences.
The Strain on Provider-Patient Relationships
Incorrect billing and inaccurate coding can lead to disputes between patients and healthcare providers. Patients who are incorrectly billed may become frustrated and lose faith in their healthcare providers, damaging the professional relationship and potentially leading them to seek care elsewhere.
Impact on Quality of Care
Focusing on addressing inaccurate coding and billing errors may draw resources away from patient care, potentially compromising the quality of care provided by healthcare institutions. Providers may focus more on addressing these issues, leading to decreased attention to direct patient care.
Inaccurate coding and billing can have far-reaching consequences for healthcare providers. These pitfalls can result in financial losses, legal matters, loss of reputation, potential audits and investigations, strained provider-patient relationships, and compromised quality of care.
Loss of Accreditation
When a patient is inaccurately coded it can raise concerns about the authenticity of the physician, healthcare practice, coder, and the. For example, when there’s no correlation found between the diagnosis and the treatment provided, it can raise questions about the authorization of the parties concerned.
Most specifically, the provider and then the coder and biller are brought under inspection for the errors made. If your practice has experienced any such consequences, outsourcing your medical billing and coding to Bellmedex can be a great way to fix these errors.
Effects on Medical Research
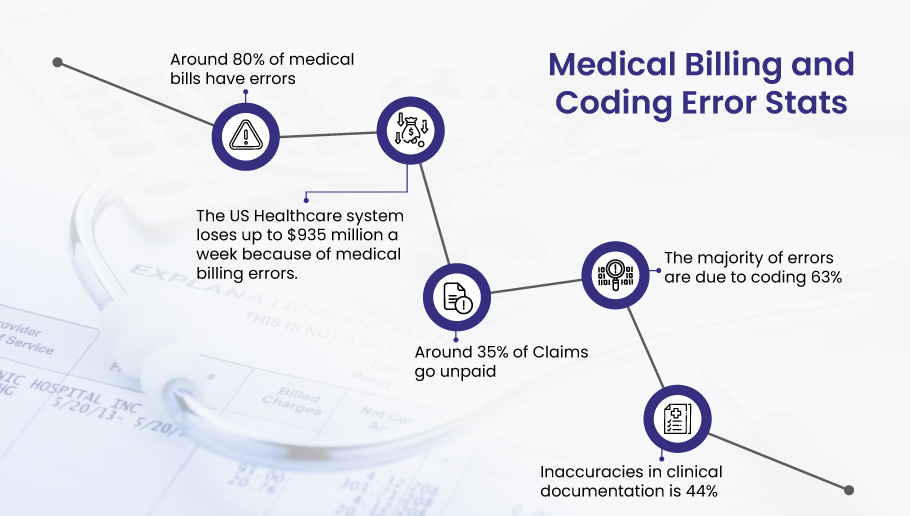
Studies indicate that around 80% of medical bills have errors. Inaccuracy in coding and billing directly affects medical research. When patients are wrongly coded, consequently, the data collected is false. This can lead to incorrect reports and research in the medical field thus, negatively impacting the overall trends and patterns in medical research.
Negative Influence on Healthcare Policy
Healthcare policy is a crucial aspect of the US Healthcare system. Without it, the wellbeing of the masses is not possible and the system can collapse at any moment. It’s important to note that inaccurate coding and billing have a huge impact on healthcare policy. Every healthcare practice has certain policies that they have to abide by. For instance, the laws, regulations, and actions against scams and fraudulent activities. False coding and billing negatively influence the healthcare policy of providing overall wellness and quality care to their patients.
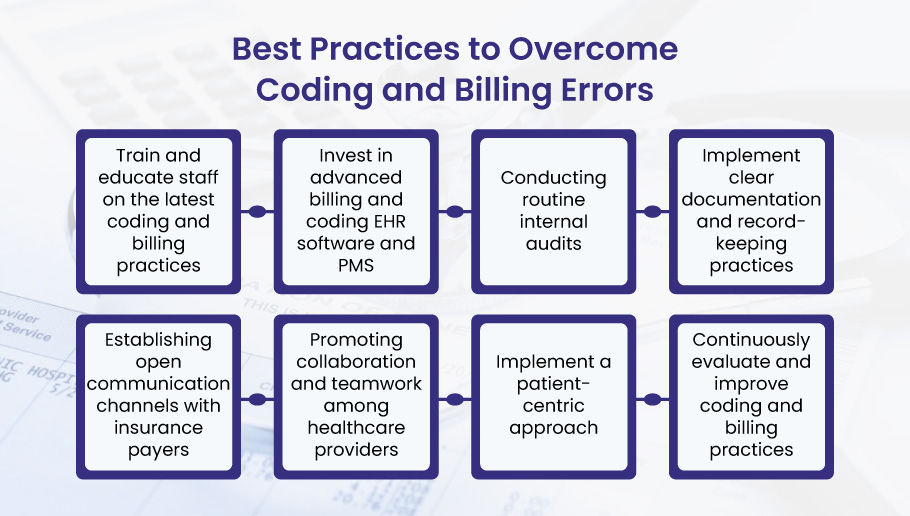
Best Practices to Overcome Inaccurate Coding and Incorrect Billing
Providers should adopt best practices that promote accurate and efficient processes to overcome the challenges associated with inaccurate coding and billing in healthcare. Let’s discuss various strategies to help healthcare institutions prevent medical abuse, fraud, and the negative consequences of billing errors.
- Train and educate staff on the latest coding and billing practices i.e. ICD-10 and ICD-11, regulations, and updates to ensure that the team is well-equipped for coding and billing.
- Invest in advanced billing and coding EHR software and PMS, that automatically flags errors and inconsistencies. This allows healthcare providers to correct mistakes.
- Conducting routine internal audits allows healthcare providers to rectify mistakes before they become more significant problems.
- Implement clear documentation and record-keeping practices to maintain accurate patient records, which is vital for ensuring accurate coding and billing.
- Establishing open communication channels with insurance payers helps address coding or billing discrepancies. This fosters a cooperative relationship and can help prevent delays or denials in reimbursement.
- Promoting collaboration and teamwork among healthcare providers allows for a more comprehensive approach to ensuring accurate coding and billing and can lead to the identification of potential errors.
- Make sure to implement a patient-centric approach to promote trust and transparency between healthcare providers and their patients.
- It’s essential to continuously evaluate and improve coding and billing practices such as updating procedures, or investing in new technology to streamline the billing and coding process.
By adopting these best practices, healthcare providers can effectively overcome the challenges of inaccurate coding and billing. Doing so can help prevent medical abuse, fraud, and financial penalties while fostering patient trust and promoting the overall quality of care.
Conclusion
Studies indicate that around 80% of medical bills have errors. Inaccuracy in coding and billing directly affects medical research. When patients are wrongly coded, consequently, the data collected is false. This can lead to incorrect reports and research in the medical field thus, negatively impacting the overall trends and patterns in medical research.
If you’re looking to outsource your medical coding and billing services, make sure you get advanced automation, real-time error checking, up-to-date coding guidelines, claims scrubbing, integration with EHR/EMR systems, advanced analytics, audit trail, and elimination of DRG coding errors. At Bellmedex we ensure all your medical billing and coding is efficiently done and taken care of along with the above-mentioned services.
By investing in Bellmedex, healthcare providers can significantly reduce the likelihood of inaccurate coding and billing, safeguarding financial stability, reputation, and patient trust. Ultimately, this will lead to improved quality of care and a more efficient healthcare system for healthcare providers.